The Reproductive Physiology
Sexual Reproduction is the biological process through which organisms produce offspring by combining genetic material from two distinct gametes: the male gamete (sperm cell) and the female gamete (secondary oocyte).
- Fertilization: The union of a sperm cell with a secondary oocyte results in a zygote containing a complete set of chromosomes—half from each parent.
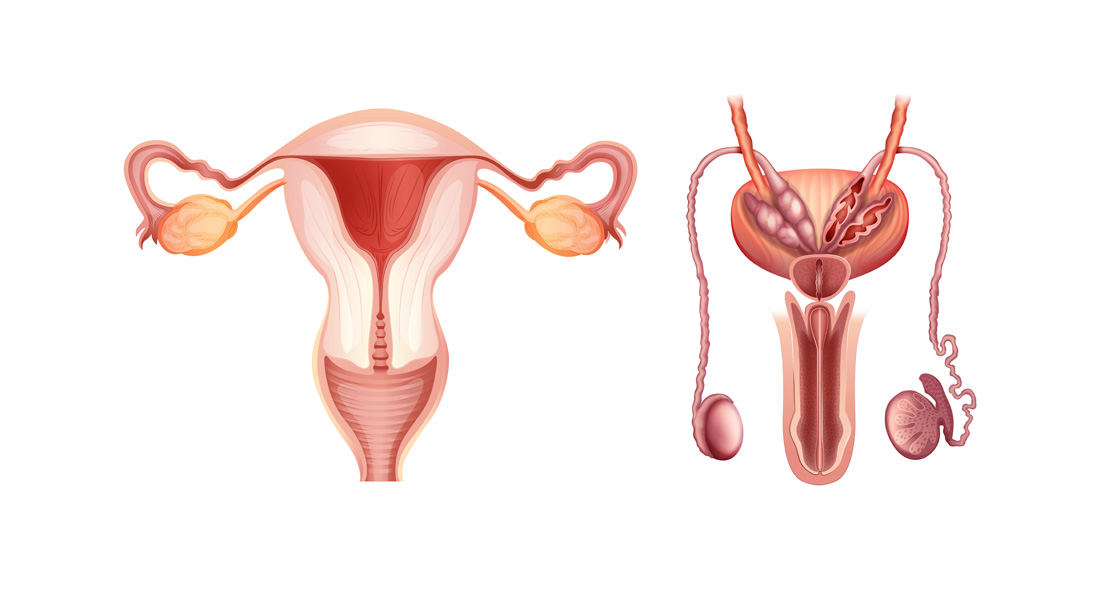
- Anatomical Distinctions: Males and females possess distinct reproductive organs tailored for:
- Producing gametes
- Facilitating fertilization
- Sustaining embryonic and fetal growth (in females)
Reproductive Systems Overview
Male Reproductive System
Components:
- Testes (Male Gonads)
- Produce sperm (gametes)
- Secrete hormones (e.g., testosterone)
- Duct System
- Epididymis: Stores and matures sperm
- Ductus Deferens: Transports sperm from epididymis
- Ejaculatory Ducts: Convey sperm to urethra
- Urethra: Pathway for sperm to exit the body
- Accessory Sex Glands
- Seminal Vesicles: Produce seminal fluid rich in fructose
- Prostate Gland: Secretes a fluid that nourishes and protects sperm
- Bulbourethral Glands: Produce pre-ejaculate fluid
- Supporting Structures
- Scrotum: Houses and protects the testes; regulates temperature for optimal sperm production
- Penis: Facilitates the delivery of sperm into the female reproductive tract
Female Reproductive System
Components:
- Ovaries (Female Gonads)
- Produce oocytes (gametes)
- Secrete hormones (e.g., estrogen, progesterone)
- Uterine (Fallopian) Tubes/Oviducts
- Transport oocytes from ovaries to the uterus
- Site of fertilization
- Uterus
- Houses and nurtures the developing embryo and fetus
- Houses and nurtures the developing embryo and fetus
- Vagina
- Receives sperm during copulation
- Serves as the birth canal
Spermatogenesis: Formation of Sperm
Location: Seminiferous Tubules within the testes
Process Duration: 65–75 days in humans
Stages of Spermatogenesis
-
Spermatogonia (Stem Cells)
- Type: Diploid (2n; 46 chromosomes)
- Function: Undergo mitosis to produce more spermatogonia or differentiate into primary spermatocytes
- Location: Near the basement membrane of seminiferous tubules
-
Primary Spermatocytes
- Type: Diploid (2n; 46 chromosomes)
- Process:
- DNA replication occurs prior to meiosis
- Undergo Meiosis I to form secondary spermatocytes
-
Secondary Spermatocytes
- Type: Haploid (n; 23 chromosomes)
- Structure: Each chromosome consists of two chromatids
- Process:
- Undergo Meiosis II to form spermatids
- Undergo Meiosis II to form spermatids
-
Spermatids
- Type: Haploid (n; 23 chromosomes)
- Process: Undergo Spermiogenesis to transform into mature sperm cells
-
Spermiogenesis
- Description: Differentiation of spermatids into elongated, motile spermatozoa
- Outcome: Formation of mature sperm with distinct head and tail structures
- Event: Spermiation – release of mature sperm into the lumen of seminiferous tubules
Sperm Structure
-
Head
- Size: Approximately 4–5 μm long
- Components:
- Nucleus: Contains 23 condensed chromosomes
- Acrosome: Cap-like vesicle filled with enzymes (e.g., hyaluronidase, proteases) essential for penetrating the secondary oocyte
-
Tail
- Components:
- Neck: Contains centrioles essential for tail formation
- Middle Piece: Packed with mitochondria arranged in a spiral to provide ATP for motility
- Principal Piece: Longest segment, responsible for the whip-like movement
- End Piece: Tapers off at the terminal end
- Components:
Daily Sperm Production: Approximately 300 million sperm are produced each day.
Hormonal Control of the Testes
Regulatory Axis: Hypothalamus → Anterior Pituitary → Testes
-
Gonadotropin-Releasing Hormone (GnRH)
- Source: Hypothalamic neurosecretory cells
- Function: Stimulates the anterior pituitary to secrete gonadotropins
-
Gonadotropins
- Luteinizing Hormone (LH)
- Target: Leydig cells in testes
- Function: Stimulates secretion of testosterone
- Follicle-Stimulating Hormone (FSH)
- Target: Sertoli cells in testes
- Function: Promotes spermatogenesis and secretion of androgen-binding protein (ABP)
- Luteinizing Hormone (LH)
-
Testosterone
- Source: Leydig cells
- Function:
- Development and maintenance of male secondary sexual characteristics
- Supports spermatogenesis
- Acts via negative feedback to inhibit GnRH and LH secretion
-
Androgen-Binding Protein (ABP)
- Source: Sertoli cells
- Function: Binds testosterone to maintain high local concentrations necessary for spermatogenesis
-
Inhibin
- Source: Sertoli cells
- Function: Inhibits FSH secretion via negative feedback
Feedback Mechanism
- Negative Feedback: Elevated testosterone levels inhibit GnRH and LH secretion, maintaining hormonal balance.
Roles of Androgens
-
Prenatal Development
- Testosterone: Stimulates male duct development and testicular descent
- Dihydrotestosterone (DHT): Promotes external genitalia formation
-
Pubertal Development
- Testosterone & DHT: Induce growth and enlargement of male reproductive organs and development of secondary sexual characteristics (e.g., facial hair, deepening voice)
- Testosterone & DHT: Induce growth and enlargement of male reproductive organs and development of secondary sexual characteristics (e.g., facial hair, deepening voice)
-
Adult Functions
- Sexual Behavior: Influences libido and sexual drive
- Anabolic Effects: Promote protein synthesis and muscle growth
Female Reproductive Physiology
Female Reproductive Cycle
Phases:
- Ovarian Cycle
- Events: Maturation of oocytes and hormone secretion
- Uterine (Menstrual) Cycle
- Events: Preparation of the endometrium for implantation
Cycle Duration: Approximately one month (28 days)
Phases of the Ovarian Cycle
-
Menstrual Phase (Days 1–5)
- Events:
- Shedding of the stratum functionalis of the endometrium if fertilization does not occur
- Menstrual flow: 50–150 mL of blood and cellular debris
- Hormonal Changes:
- Declining progesterone and estrogen levels
- Release of prostaglandins causing vasoconstriction and cell death in the endometrium
- Events:
-
Preovulatory Phase (Days 6–14) – Proliferative Phase
- Events:
- Follicular growth stimulated by FSH
- Selection of a dominant follicle
- Maturation of the dominant (graafian) follicle
- Proliferation and thickening of the endometrium under estrogen influence
- Hormonal Changes:
- Increased estrogen and inhibin from the dominant follicle
- Negative feedback reduces FSH levels, inhibiting growth of other follicles
- Events:
-
Ovulation (Around Day 14)
- Events:
- Rupture of the mature graafian follicle
- Release of the secondary oocyte into the pelvic cavity
- Possible pain (mittelschmerz) due to follicle rupture
- Hormonal Changes:
- Positive feedback from high estrogen levels triggers a surge in LH and GnRH
- LH surge induces ovulation
- Events:
-
Postovulatory Phase (Days 15–28) – Luteal Phase
- Events:
- Transformation of the ruptured follicle into the corpus luteum
- Secretion of progesterone, estrogen, relaxin, and inhibin by the corpus luteum
- Preparation of the endometrium for potential implantation (secretory phase)
- Hormonal Changes:
- Progesterone and estrogen exert negative feedback on GnRH, LH, and FSH
- If fertilization does not occur, corpus luteum degenerates into corpus albicans
- Decline in progesterone and estrogen leads to menstruation
- Events:
Hormonal Regulation of the Female Reproductive Cycle
-
Gonadotropin-Releasing Hormone (GnRH)
- Source: Hypothalamus
- Function: Stimulates anterior pituitary to release FSH and LH
-
Follicle-Stimulating Hormone (FSH)
- Function: Initiates follicular growth in ovaries
- Mechanism: Granulosa cells convert androgens to estrogens under FSH influence
-
Luteinizing Hormone (LH)
- Function: Triggers ovulation and stimulates corpus luteum formation
- Mechanism: Promotes secretion of progesterone and estrogen from the corpus luteum
-
Estrogens
- Sources: Ovarian follicles and corpus luteum
- Functions:
- Development and maintenance of female reproductive structures
- Promotion of secondary sex characteristics (e.g., breast development)
- Enhancement of protein anabolism and bone strength
- Inhibition of GnRH, LH, and FSH at high levels
-
Progesterone
- Source: Corpus luteum
- Functions:
- Prepares and maintains the endometrium for implantation
- Inhibits GnRH and LH secretion at high levels
- Prepares mammary glands for milk secretion
-
Relaxin
- Source: Corpus luteum and placenta (during pregnancy)
- Functions:
- Relaxes uterine smooth muscle to facilitate implantation and pregnancy
- Increases flexibility of pubic symphysis and dilates the cervix during labor
-
Inhibin
- Source: Granulosa cells and corpus luteum
- Function: Inhibits FSH secretion through negative feedback
Ovarian and Uterine Cycle Coordination
- Ovarian Cycle: Involves the maturation of the oocyte and hormonal changes in the ovary.
- Uterine (Menstrual) Cycle: Involves cyclical changes in the endometrium to prepare for potential implantation.
Detailed Phases of the Female Reproductive Cycle
1. Menstrual Phase (Days 1–5)
- Follicular Development:
- Under FSH influence, primordial follicles develop into primary and then secondary follicles.
- Note: Follicular maturation can span several menstrual cycles; not all developing follicles reach ovulation.
- Endometrial Changes:
- Decline in progesterone and estrogen leads to vasoconstriction of uterine spiral arterioles.
- Resulting hypoxia causes cell death and shedding of the stratum functionalis.
- Menstrual Flow: Composed of blood, tissue fluid, mucus, and epithelial cells.
2. Preovulatory Phase (Days 6–14) – Proliferative Phase
- Dominant Follicle Selection:
- Among developing follicles, one becomes dominant due to better responsiveness to FSH.
- Hormonal Influence:
- Dominant follicle secretes estrogens and inhibin, inhibiting FSH and preventing further follicular growth.
- Endometrial Proliferation:
- Estrogens stimulate mitosis in the stratum basalis, regenerating the stratum functionalis.
- Development and thickening of endometrial glands and blood vessels.
- Corpus Luteum Formation:
- As the dominant follicle matures, it prepares for potential ovulation.
3. Ovulation (Around Day 14)
- Process:
- LH surge induced by positive feedback from high estrogen levels.
- LH causes rupture of the mature graafian follicle, releasing the secondary oocyte.
- Post-Ovulation:
- Oocyte enters the uterine tube, surrounded by zona pellucida and corona radiata cells.
- Potential for fertilization occurs within the uterine tube.
- Clinical Note:
- Mittelschmerz: Ovulation pain due to follicle rupture.
- Ovulation Prediction: Home LH tests can predict ovulation by detecting LH surge.
4. Postovulatory Phase (Days 15–28) – Luteal Phase
-
Corpus Luteum Formation:
- Ruptured follicle transforms into corpus luteum (via corpus hemorrhagicum)
- Hormones Secreted: Progesterone, estrogen, relaxin, inhibin
-
Endometrial Preparation:
- Secretory Phase: Progesterone and estrogen enhance endometrial glands to secrete nutrients (e.g., glycogen)
- Endometrial Thickening: Up to 12–18 mm to support potential implantation
-
If Fertilization Occurs:
- Corpus Luteum Maintenance: Rescued by human chorionic gonadotropin (hCG) produced by the embryo
- Pregnancy Support: Corpus luteum continues hormone secretion to sustain the endometrium
-
If Fertilization Does Not Occur:
- Corpus Luteum Degeneration: Transforms into corpus albicans
- Hormonal Decline: Decreased progesterone and estrogen lead to menstrual phase initiation
Summary of Hormonal Regulation
- Hypothalamus secretes GnRH → stimulates anterior pituitary to release FSH and LH
- FSH: Promotes follicular growth and estrogen secretion
- LH: Triggers ovulation and corpus luteum formation; stimulates testosterone production in males
- Estrogens and Progesterone: Regulate endometrial changes and exert feedback on GnRH, FSH, and LH
- Inhibin: Specifically inhibits FSH secretion
Key Concepts
- Negative Feedback: Maintains hormonal balance by regulating hormone secretion based on current levels (e.g., testosterone in males, estrogens and progesterone in females)
- Positive Feedback: Occurs during ovulation where high estrogen levels lead to a surge in LH
- Anabolic Effects of Androgens: Promote growth and protein synthesis, contributing to secondary sexual characteristics
- Role of ADH and Relaxin: While ADH is more associated with kidney function, relaxin plays a critical role in the female reproductive system by preparing the uterus for pregnancy and childbirth
Important Terms
- Gamete: Reproductive cell (sperm in males, oocyte in females)
- Meiosis: Type of cell division that reduces chromosome number by half, producing haploid cells
- Spermiogenesis: Process of sperm maturation without cell division
- Corpus Luteum: Temporary endocrine structure involved in the production of progesterone
- Corpus Albicans: Degenerated corpus luteum post non-fertilization
- hCG (Human Chorionic Gonadotropin): Hormone produced during pregnancy, detected by pregnancy tests
Clinical Relevance
- Ovulation Prediction: LH surge detection helps in family planning and fertility treatments
- Menstrual Disorders: Imbalances in hormonal regulation can lead to irregular cycles, amenorrhea, or dysmenorrhea
- Infertility: Disruptions in spermatogenesis or oogenesis, hormonal imbalances, or anatomical issues can affect fertility
- Hormonal Therapies: Used in contraceptives, hormone replacement therapies, and treatment of reproductive disorders


Free Videos