The Urinary System
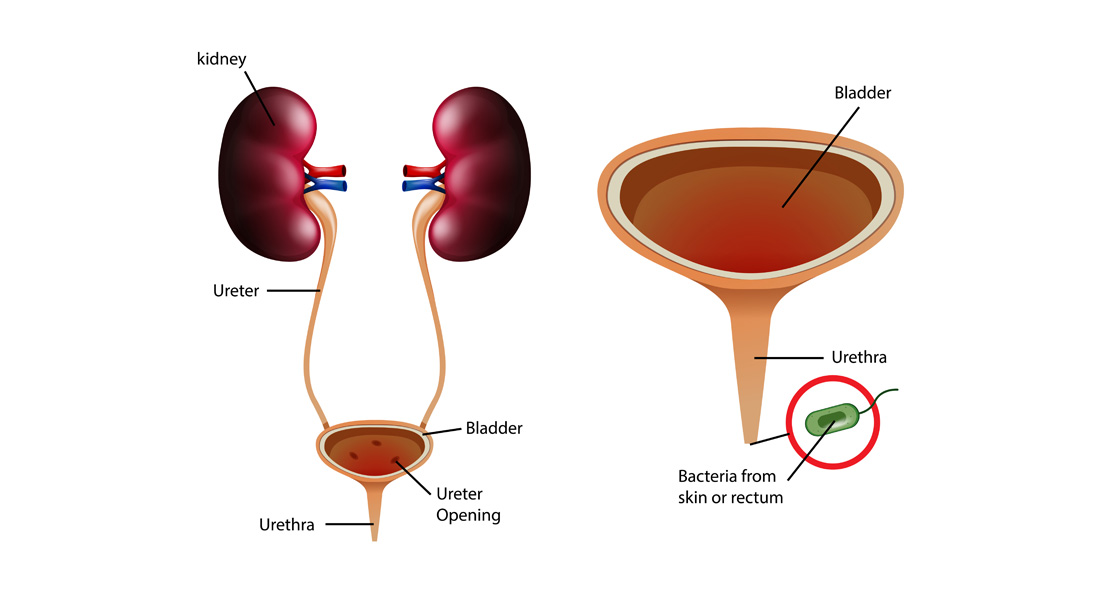
The urinary system is one of the body's primary excretory systems, responsible for removing waste products and maintaining fluid and electrolyte balance. It includes the following key components:
- Kidneys
- Ureters
- Urinary bladder
- Urethra
Besides the urinary system, three other systems contribute to excretion: the bowel, lungs, and skin.
Functions of the Urinary System:
- The kidneys filter waste products of metabolism, excess water, and salts from the blood and maintain the pH balance.
- The ureters carry urine from the kidneys to the bladder.
- The urinary bladder serves as a reservoir for urine.
- The urethra facilitates the excretion of urine to the exterior.
The Kidneys (Renes)
Definition: The kidneys are a pair of excretory organs located on the posterior abdominal wall, one on either side of the vertebral column, behind the peritoneum.
Location:
- Occupies the epigastric, hypochondriac, lumbar, and umbilical regions.
- Extends vertically from the upper border of the 12th thoracic vertebra to the center of the 3rd lumbar vertebra.
- The right kidney is slightly lower than the left due to the position of the liver. The left kidney is also nearer to the median plane than the right.
Surface Anatomy:
- External Features: Each kidney is bean-shaped with the following features:
- Poles: Upper and lower poles. The upper pole is broad and in contact with the suprarenal gland; the lower pole is pointed.
- Borders: Lateral (convex) and medial (concave). The middle part of the medial border is depressed and is known as the hilum, where structures enter and leave the kidney.
- Surfaces: Anterior and posterior.
Measurements:
- Color: Reddish-brown.
- Length: ~11 cm (left kidney is slightly longer and narrower than the right).
- Width: ~6 cm.
- Thickness: ~3 cm.
- Weight:
- Males: ~150 gm.
- Females: ~135 gm.
- Note: In fetuses, the kidney is lobulated, made up of about 12 lobules that fuse after birth, giving the kidney its smooth appearance in adults.
Surface Marking:
- The Morris parallelogram is used for the surface marking of the kidney.
Coverings:
The kidneys are protected by three layers:
- Innermost fibrous capsule (true capsule).
- Middle fatty capsule (perinephric fat) – acts as a shock absorber and helps maintain the kidney's position.
- False capsule (renal fascia) – consists of two layers (anterior and posterior), which merge with the diaphragmatic fascia and are responsible for kidney movement during respiration.
Anatomy of the Kidney
Macroscopic Structure:
- Renal Capsule: The outer protective layer.
- Renal Cortex: The outer 1 cm thick layer of the kidney.
- Renal Medulla: The inner part that consists of renal columns and renal pyramids.
- Renal Pyramids: Triangular structures whose tips (papillae) point towards the renal pelvis.
- Renal Pelvis: A funnel-shaped structure where urine is collected.
- Calyces: Minor calyces collect urine from the papillae, which then combine to form major calyces that drain into the renal pelvis.
Microscopic Structure (Histology):
- The kidney consists of millions of uriniferous tubules, which are made up of nephrons (the functional unit of the kidney) and collecting tubules.
- Each kidney has over 1 to 2 million nephrons and thousands of collecting ducts.
Nephron:
- The nephron consists of the glomerulus, Bowman’s capsule, proximal convoluted tubule, loop of Henle, distal convoluted tubule, and collecting duct.
- Key processes include filtration, reabsorption, and secretion, ensuring that waste is excreted and useful substances are reabsorbed into the bloodstream.
Functions of the Kidney
- Filtration: The kidney filters blood plasma, removing waste products and returning useful chemicals to the blood.
- Regulation of blood volume and pressure: Through the renin-angiotensin-aldosterone system (RAAS), which controls blood pressure and electrolyte balance.
- Osmoregulation: Maintains the osmolarity of body fluids.
- Erythropoiesis: Secretes erythropoietin, a hormone that regulates red blood cell production.
- Acid-base balance: Regulates partial pressure of CO₂ (PCO₂) and maintains acid-base balance.
- Detoxification: Detoxifies free radicals and drugs.
- Gluconeogenesis: Produces glucose from non-carbohydrate sources during periods of fasting.
Blood Supply to the Kidneys
- Arterial Supply: The kidneys receive blood from the renal arteries, which branch directly from the abdominal aorta.
- Venous Drainage: The kidneys drain blood through the renal veins, which terminate in the inferior vena cava. The left renal vein is longer than the right.
- Nerve Supply: Sympathetic fibers are derived from the T10-L1 segments, and parasympathetic fibers come from the vagus nerve.
- Lymphatic Drainage: Drains into the lateral aortic nodes.
The Ureters
Definition:
The ureters are two narrow, thick-walled muscular tubes that convey urine from the kidneys to the bladder.
Dimensions:
- Length: ~25 cm (10 inches).
- Diameter: ~3 mm, but constrictions are present at three points:
- Pelviureteric junction
- Brim of the lesser pelvis
- Passage through the bladder wall
Parts:
- Abdominal part: From the origin to the pelvic brim.
- Pelvic part: From the pelvic brim to the entry into the bladder.
Cross-Section Structure:
- Outer layer: Fibrous tissue.
- Middle layer: Muscle.
- Inner layer: Epithelium.
Blood Supply:
- Supplied by branches of the renal artery, abdominal aorta, gonadal artery, common iliac artery, internal iliac artery, and inferior vesical artery.
Nerve Supply:
- Controlled by the autonomic nervous system.
Urinary Bladder
Definition:
The urinary bladder is a hollow, muscular organ that stores urine and periodically discharges it.
Position:
- In an empty state, the bladder lies within the pelvis. When distended, it extends into the abdominal cavity.
Capacity:
- The mean capacity is about 220 ml. Filling beyond this causes the urge to urinate. Toleration may extend up to 500 ml, but this becomes painful.
Shape:
- When empty, the bladder resembles a four-sided pyramid, with four surfaces:
- Base (posterior surface)
- Inferolateral surfaces (2)
- Superior surface
Structure:
- Outer layer: Loose connective tissue.
- Middle layer: Smooth muscle and elastic fibers.
- Inner layer: Lined with transitional epithelium.
- Interior: The mucous membrane is thrown into folds, except in the trigone (a smooth triangular area at the posterior wall with no folds).
The Urethra
Definition:
The urethra is a canal that extends from the neck of the bladder to the exterior. Its length differs between males and females:
- Male urethra: ~20 cm (8 inches).
- Female urethra: ~3-4 cm (1.5 inches).
Applied Anatomy:
- The shorter female urethra is a factor in the higher frequency of urinary tract infections (UTIs) in females, as bacteria from the stool can more easily ascend into the urinary system.
Female Urethra:
- External urethral orifice: Located between the vaginal orifice and clitoris.
- Internal urethral sphincter: Smooth muscle under involuntary control.
- External urethral sphincter: Skeletal muscle under voluntary control.
Male Urethra:
- Comprises three regions:
- Prostatic urethra: Receives semen during ejaculation.
- Membranous urethra: Passes through the pelvic cavity.
- Penile urethra: Extends through the penis.
Applied Anatomy of the Urinary System
Congenital Anomalies:
- Unilateral/Bilateral Agenesis: Absence of one or both kidneys.
- Horseshoe Kidney: Fusion of the lower poles of the kidneys.
- Congenital Polycystic Disease: Formation of multiple cysts.
- Ectopic Kidney: Kidney located in an abnormal position.
- Abnormal Renal Arteries: Renal arteries may arise from the aorta or superior mesenteric artery.
Infections:
- Cystitis: Bladder infection.
Other Conditions:
- Renal failure: Inability of the kidneys to perform their essential functions.
- Bladder rupture, neurological lesions, bladder cancer, and urinary incontinence.


Free Videos