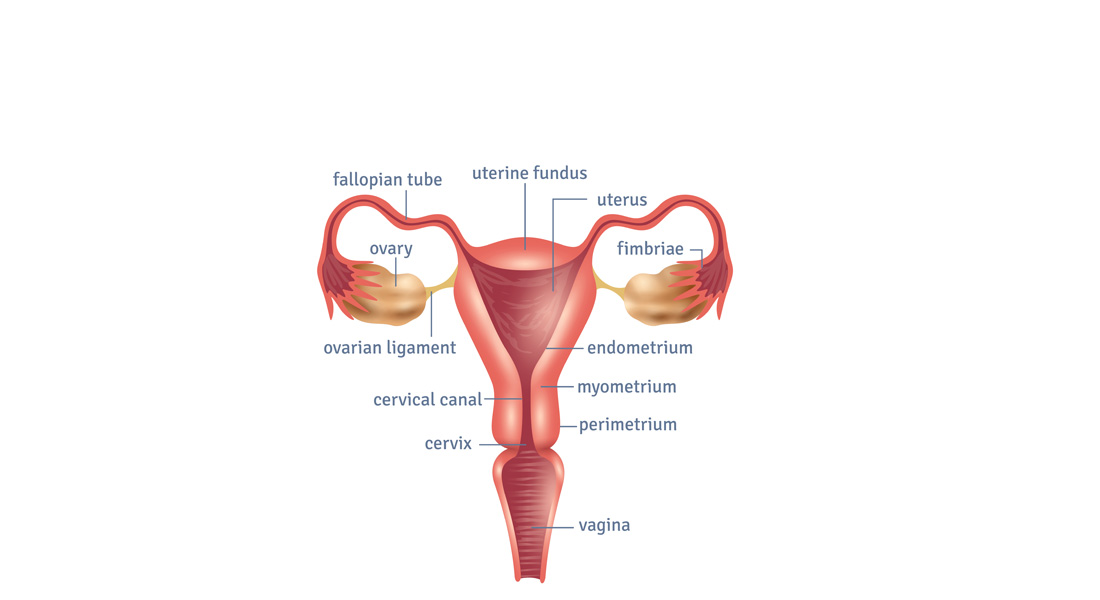
Female Reproductive System
The female reproductive system is a complex network of organs and structures that play essential roles in reproduction, hormone production, and overall female health.
- Complex Role:
- The reproductive role of a female is more intricate than that of a male. Apart from producing gametes (ova), the female body also prepares to nurture a fetus for approximately nine months.
- Primary Reproductive Organs:
- Ovaries are the female gonads and serve two main functions:
- Producing female gametes (ova).
- Secreting sex hormones, estrogen and progesterone.
- Ovaries are the female gonads and serve two main functions:
Divisions of the Female Reproductive System
-
Internal Genitalia:
- Includes the ovaries and the duct system, primarily located in the pelvic cavity.
- Accessory Ducts: Include uterine tubes, uterus, and vagina, which transport gametes and support fetal development.
-
External Genitalia:
- Refers to the sex organs located outside the body, commonly referred to as the vulva.
Ovaries
-
Location and Size:
- The ovaries are paired, oval-shaped organs located on either side of the uterus, measuring about 2 cm in length and 1 cm in width.
- The ovaries are paired, oval-shaped organs located on either side of the uterus, measuring about 2 cm in length and 1 cm in width.
-
Functions:
- Gamete Production: Produces oocytes (female gametes).
- Hormone Secretion: Produces estrogen and progesterone in response to pituitary hormones (LH and FSH).
-
Egg Supply:
- A female is born with approximately 1-2 million eggs, but only about 300 will mature and be ovulated for fertilization over her lifetime.
- A female is born with approximately 1-2 million eggs, but only about 300 will mature and be ovulated for fertilization over her lifetime.
-
Structure:
- Surface: Covered by germinal epithelium, a simple cuboidal epithelium.
- Cortex: The outer region, made of connective tissue stroma, which contains numerous primordial follicles housing immature eggs.
- Medulla: The inner region, composed of supportive stroma and rich in blood vessels and nerves.
Ligaments of the Ovary
-
Suspensory Ligament:
- Extends from the ovary to the pelvic wall, containing neurovascular structures.
- Extends from the ovary to the pelvic wall, containing neurovascular structures.
-
Ovarian Ligament:
- Connects the ovary to the uterus and continues as the round ligament.
Blood Supply and Nerve Supply to the Ovaries
-
Arterial Supply:
- The ovaries receive blood from the ovarian arteries, which originate from the abdominal aorta, and from the uterine arteries.
- The ovaries receive blood from the ovarian arteries, which originate from the abdominal aorta, and from the uterine arteries.
-
Venous Drainage:
- The right ovarian vein drains into the inferior vena cava, while the left ovarian vein drains into the left renal vein.
- The right ovarian vein drains into the inferior vena cava, while the left ovarian vein drains into the left renal vein.
-
Nerve Supply:
- Ovaries receive both sympathetic and parasympathetic innervation via the ovarian and uterine plexuses, which enter through the suspensory ligament.
- Ovaries receive both sympathetic and parasympathetic innervation via the ovarian and uterine plexuses, which enter through the suspensory ligament.
-
Lymphatic Drainage:
- Lymph from the ovaries drains into the para-aortic lymph nodes.
Uterine (Fallopian) Tubes
- Function:
- The uterine tubes (also known as fallopian tubes or oviducts) are responsible for transporting the ovulated egg from the ovary to the uterus, and they provide the site for fertilization.
- Anatomy:
- The uterine tubes are approximately 10 cm long and divided into several sections:
- Fimbriae: Finger-like projections that capture the ovum.
- Infundibulum: A funnel-shaped structure attached to the fimbriae.
- Ampulla: The widest section, where fertilization usually occurs.
- Isthmus: A narrow segment that connects the ampulla to the uterus.
- Interstitial Segment: Extends from the uterine cavity through the muscle of the uterus.
- The uterine tubes are approximately 10 cm long and divided into several sections:
Histology of Uterine Tubes
-
The inner lining of the uterine tubes is made up of:
- Ciliated Cells: Move the ovum or fertilized zygote toward the uterus by sweeping motions.
- Peg Cells: Non-ciliated secretory cells that provide nutrients to the ovum.
-
Smooth Muscle:
- The smooth muscle layer in the uterine tubes contracts to facilitate the movement of both the egg and sperm. This activity is influenced by sex hormones, particularly estrogen.
Vascular and Nervous Supply to Uterine Tubes
-
Blood Supply:
- The arterial supply comes from both the uterine and ovarian arteries.
- Venous drainage occurs via the uterine and ovarian veins.
-
Lymphatic Drainage:
- Lymph from the uterine tubes drains into the iliac, sacral, and aortic lymph nodes.
- Lymph from the uterine tubes drains into the iliac, sacral, and aortic lymph nodes.
-
Nerve Supply:
- The uterine tubes are innervated by sympathetic and parasympathetic fibers from the ovarian and uterine (pelvic) plexuses.
- Sensory nerves travel along spinal nerves T11-L1.
The Uterus
-
Function:
- The uterus, also known as the womb, is a hollow organ responsible for holding and nurturing a fetus during pregnancy.
- It plays a crucial role in fertility and childbearing, capable of changing shape as its muscles contract and relax to accommodate a growing fetus.
- Located anterior to the rectum and posterosuperior to the bladder in the pelvis.
-
Classification:
- The uterus is considered a secondary sex organ that matures during puberty under the influence of sex hormones from the primary sex organs (ovaries).
- It is responsible for the maintenance and transportation of gametes and plays a critical role in the reproductive process.
Structure of the Uterus
- The uterus has three main parts:
- Fundus: The uppermost part, above the entry point of the uterine tubes.
- Body: The central region, where implantation of the blastocyst typically occurs.
- Cervix: The lower portion that connects the uterus to the vagina, distinct in structure and function.
Histological Structure of the Uterus
The fundus and body of the uterus consist of three tissue layers:
-
Peritoneum (Perimetrium):
- The outermost double-layered membrane, continuous with the abdominal peritoneum.
- The outermost double-layered membrane, continuous with the abdominal peritoneum.
-
Myometrium:
- The thick, muscular layer of the uterus.
- Undergoes hypertrophy and hyperplasia during pregnancy to prepare for childbirth.
-
Endometrium:
- The innermost mucous membrane lining the uterus.
- Divided into two layers:
- Stratum Basalis: The deeper layer that remains constant throughout the menstrual cycle and regenerates the functional layer after menstruation.
- Stratum Functionalis: The superficial layer that responds to hormones and is shed during menstruation if no implantation occurs.
Endometrial Phases
- Proliferative Phase:
- Glands and blood vessels scatter through the functional zone with little branching. New glands form and the endometrium thickens.
- Secretory Phase:
- Glands enlarge and branch, preparing the endometrium for implantation.
- If no implantation occurs, the endometrium breaks down, initiating menstruation.
Position of the Uterus
- The position of the uterus varies based on bladder distension.
- In most adult women, the uterus is:
- Anteverted: Tilted forward towards the front of the body.
- Anteflexed: Flexed forward relative to the cervix.
- It typically lies posterosuperior to the bladder and anterior to the rectum.
Ligaments Supporting the Uterus
Several ligaments provide support to the uterus and help maintain its position:
-
Broad Ligament:
- A double layer of peritoneum that attaches the sides of the uterus to the pelvis.
- A double layer of peritoneum that attaches the sides of the uterus to the pelvis.
-
Round Ligament:
- Extends from the uterine horns to the labia majora, helping maintain the uterus in an anteverted position.
- Extends from the uterine horns to the labia majora, helping maintain the uterus in an anteverted position.
-
Ovarian Ligament:
- Connects the ovaries to the uterus.
- Connects the ovaries to the uterus.
-
Cardinal Ligament:
- Runs from the cervix to the lateral pelvic walls and contains the uterine artery and vein.
- Runs from the cervix to the lateral pelvic walls and contains the uterine artery and vein.
-
Uterosacral Ligament:
- Extends from the cervix to the sacrum, providing further support.
Blood Supply, Lymphatics, and Nerve Supply
-
Blood Supply:
- The uterine artery supplies blood to the uterus, while venous drainage occurs via a plexus in the broad ligament that drains into the uterine veins.
- The uterine artery supplies blood to the uterus, while venous drainage occurs via a plexus in the broad ligament that drains into the uterine veins.
-
Lymphatic Drainage:
- Lymphatic drainage is directed to the iliac, sacral, aortic, and inguinal lymph nodes.
- Lymphatic drainage is directed to the iliac, sacral, aortic, and inguinal lymph nodes.
-
Nerve Supply:
- Sympathetic innervation comes from the uterovaginal plexus, part of the inferior hypogastric plexus.
- Parasympathetic innervation is provided by the pelvic splanchnic nerves (S2-S4).
- Sensory nerve fibers travel via T10-T12 and L1 spinal nerves.
Cervix
-
The cervix is the narrow, lower portion of the uterus, connecting it to the vagina.
-
Structure:
- Cervical Canal: The cavity of the cervix that communicates with the vagina through the external os and the uterine body via the internal os.
- The cervix is divided into two regions:
- Ectocervix: The portion that projects into the vagina, lined with stratified squamous non-keratinized epithelium.
- Endocervical Canal: The inner portion of the cervix lined by mucus-secreting simple columnar epithelium.
Functions of the Cervix
-
Sperm Passage: The cervix facilitates the passage of sperm into the uterine cavity by dilating the external and internal os during the mid-cycle.
-
Sterility Maintenance: The cervix helps maintain the sterility of the upper female reproductive tract by preventing bacterial invasion through its mucus-secreting glands and narrow external os.
Vascular Supply and Lymphatics of the Cervix
-
Blood Supply:
- The cervix is supplied by the uterine artery, with venous drainage occurring via the uterine veins.
- The cervix is supplied by the uterine artery, with venous drainage occurring via the uterine veins.
-
Lymphatic Drainage:
- Lymph from the cervix drains into the iliac, sacral, aortic, and inguinal lymph nodes.


Free Videos