Structure and Function
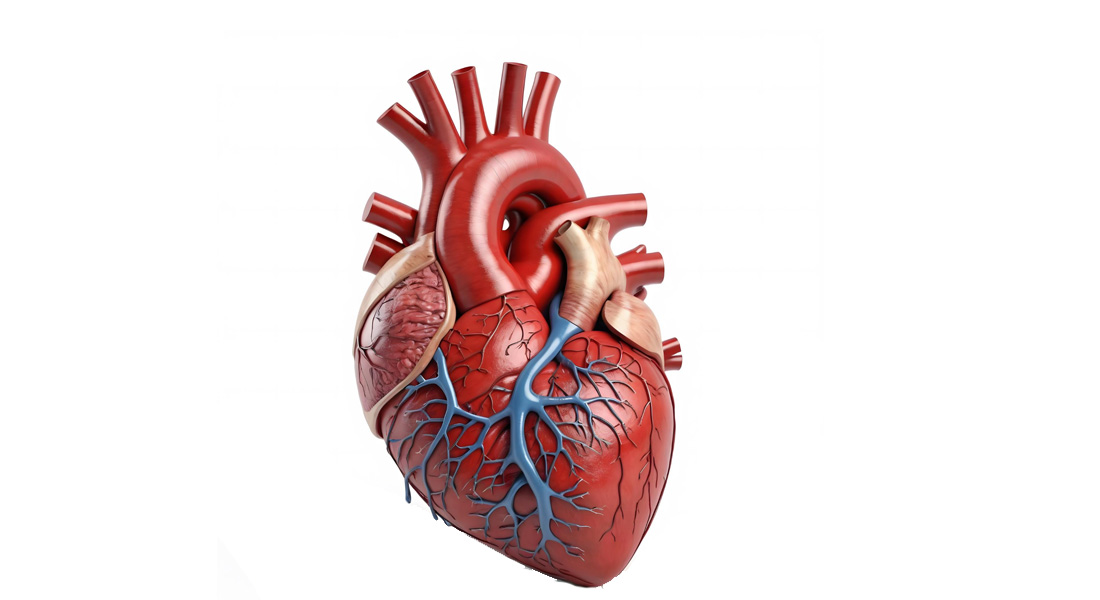
- The heart is a hollow, cone-shaped, muscular pump that is responsible for circulating blood throughout the body.
- It beats approximately 2.5 billion times in an average lifetime.
- The heart pumps blood through an extensive network of blood vessels, with the left side of the heart circulating blood through about 120,000 km of blood vessels, which is roughly equivalent to three times the Earth's equator.
- The right side of the heart pumps blood through the lungs, facilitating the exchange of gases (oxygen and carbon dioxide).
- On average, the heart pumps about 14,000 liters of blood per day, which adds up to 5 million liters per year.
Dimensions
- The heart is a relatively small organ with the following dimensions:
- Length: Approximately 12 cm (5 inches).
- Width: About 9 cm (3.5 inches) at its broadest point.
- Thickness: About 6 cm (2.5 inches).
- Mass: Around 250 g in adult females and 300 g in adult males.
- It is situated in the mediastinum, an anatomical region that extends from the sternum to the vertebral column, between the lungs.
Anatomical Relations
Superiorly
- Aorta, Superior Vena Cava, Pulmonary Artery, and Pulmonary Vein.
Inferiorly
- Diaphragm.
Anteriorly
- Ribs and Intercostal Muscles.
Posteriorly
- Esophagus, Trachea, Left and Right Bronchus, Descending Aorta, Inferior Vena Cava, and Thoracic Vertebrae.
Laterally
- Lungs.
Apex and Base
- The apex of the heart is formed by the tip of the left ventricle and rests on the diaphragm, pointing anteriorly, inferiorly, and to the left.
- The base of the heart, formed by the atria, is its posterior surface.
Heart Surfaces and Borders
Surfaces
- Sternocostal (Anterior) Surface: Located deep to the sternum and ribs.
- Diaphragmatic (Inferior) Surface: Positioned between the apex and the right border.
- Pulmonary (Left) Surface: Occupies the cardiac notch of the left lung.
Borders
- Right Border: Formed by the right atrium and faces the right lung.
- Inferior Border: Formed by the right ventricle and partly the left ventricle.
- Left Border (Pulmonary Border): Formed by the left ventricle and left auricle, facing the left lung.
- Superior Border: Formed by both atria.
Heart Sulci
- Sulci are grooves on the outer surface of the heart marking the division between the atria and ventricles.
Key Sulci
- Atrioventricular Sulcus:
- Separates the atria from the ventricles.
- Contains the right coronary artery, left coronary artery, circumflex artery, and coronary sinus.
- Anterior Interventricular Sulcus:
- Lies between the left and right ventricles on the anterior surface.
- Contains the left anterior descending artery and great cardiac vein.
- Posterior Interventricular Sulcus:
- Located between the left and right ventricles on the posterior surface.
- Contains the posterior interventricular artery and middle cardiac vein.
Pericardial Sinuses
- The pericardium forms two pericardial sinuses due to the lines of reflection between the visceral and parietal pericardium.
Types
- Transverse Pericardial Sinus:
- Positioned anterior to the superior vena cava and posterior to the ascending aorta and pulmonary trunk.
- Oblique Pericardial Sinus:
- Located posterior to the heart within the pericardial sac.
Auricles
- Each atrium's anterior surface has a wrinkled, pouch-like structure known as an auricle.
- The auricles increase the capacity of the atria, allowing them to hold a greater volume of blood.
Coverings of the Heart
- The heart is enclosed in a double-walled sac called the pericardium.
Parts of the Pericardium
-
Fibrous Pericardium:
- Tough, inelastic, dense irregular connective tissue.
- Functions to:
- Prevent overstretching of the heart.
- Protect the heart.
- Anchor the heart within the mediastinum.
-
Serous Pericardium:
- Thin, slippery, and consists of two layers:
- Parietal Layer: Fused to the fibrous pericardium.
- Visceral Layer: Also known as the epicardium, which is adhered to the surface of the heart.
- Thin, slippery, and consists of two layers:
Relationship of Serous Pericardium to the Heart
Structure and Layers
- The serous pericardium is a thinner membrane that forms a double layer around the heart.
- Outer Parietal Layer: Fused to the fibrous pericardium, providing a protective outer covering.
- Inner Visceral Layer (Epicardium): This layer adheres tightly to the surface of the heart and forms part of the heart wall.
Pericardial Cavity and Fluid
- Pericardial Fluid: A slippery fluid located between the parietal and visceral layers, providing lubrication and reducing friction as the heart beats.
- Pericardial Cavity: The space between the two layers of the serous pericardium filled with pericardial fluid.
Layers of the Heart Wall
Three Layers
-
Epicardium (External Layer):
- A thin, transparent outer layer of the heart wall composed of mesothelium (a membrane made of simple squamous cells).
- Contains blood vessels, lymphatics, and nerves that supply the myocardium.
-
Myocardium (Middle Layer):
- Responsible for the pumping action of the heart.
- Composed of cardiac muscle tissue with muscle fibers wrapped and bundled in connective tissue sheaths (endomysium and perimysium).
- The muscle fibers are organized in a circular and spiral arrangement, enhancing the strength and efficiency of the heart's pumping action.
-
Endocardium (Inner Layer):
- A glistening white sheet of endothelium (squamous epithelium) resting on a thin layer of connective tissue.
- Lines the heart chambers and covers the fibrous skeleton of the valves.
- Continuous with the endothelial linings of blood vessels entering and leaving the heart.
Chambers of the Heart
Four Chambers
- The heart has four chambers: two superior receiving chambers (atria) and two inferior pumping chambers (ventricles).
Right Atrium
- The right atrium forms the right border of the heart.
- Receives blood from the superior vena cava, inferior vena cava, and coronary sinus.
- The posterior wall is smooth, while the anterior wall has muscular ridges called pectinate muscles.
- Separated from the left atrium by the interatrial septum, which has an oval depression called the fossa ovalis.
- Blood flows from the right atrium to the right ventricle through the tricuspid valve.
Right Ventricle
- The right ventricle forms most of the anterior surface of the heart.
- Contains ridges called trabeculae carneae, which aid in heart conduction.
- Blood flows from the right ventricle through the pulmonary valve into the pulmonary trunk, which splits into the right and left pulmonary arteries.
Left Atrium
- The left atrium forms most of the base of the heart and receives oxygenated blood from the lungs through four pulmonary veins.
- Both anterior and posterior walls are smooth; pectinate muscles are confined to the auricle of the left atrium.
- Blood flows from the left atrium to the left ventricle through the bicuspid (mitral) valve.
Left Ventricle
- The left ventricle is the thickest chamber of the heart, forming the apex of the heart.
- Like the right ventricle, it contains trabeculae carneae and chordae tendineae that anchor the bicuspid valve's cusps to papillary muscles.
- Blood flows from the left ventricle through the aortic valve into the ascending aorta, which supplies the coronary arteries and the rest of the body through the arch and descending aorta.
The Valves, Blood Supply, Nerve Supply, and Cardiac Muscle Fibers
1. Valves of the Heart
Tricuspid Valve
- The tricuspid valve is located between the right atrium and the right ventricle.
- It consists of three cusps: anterior, septal, and inferior (posterior). These cusps are formed from a fold of the endocardium reinforced with connective tissue.
- The bases of the cusps attach to the fibrous ring of the heart's skeleton, and their free edges attach to the chordae tendineae. The chordae tendineae link the valve to the papillary muscles, which prevent backflow of blood during ventricular contraction.
Mitral Valve
- The mitral valve, located between the left atrium and left ventricle, has two cusps: anterior and posterior.
- The anterior cusp is larger and positioned between the atrioventricular and aortic orifices.
- Like the tricuspid valve, the cusps are anchored to papillary muscles via chordae tendineae, which prevent prolapse during ventricular contraction.
Pulmonary Valve
- The pulmonary valve lies between the right ventricle and the pulmonary trunk.
- It has three semilunar cusps formed by folds of the endocardium with connective tissue. These cusps lack chordae tendineae or papillary muscles.
- The cusps are named anterior (AC), left (LC), and right (RC).
Aortic Valve
- Located between the left ventricle and the aorta, the aortic valve has three cusps: left coronary cusp (LCC), right coronary cusp (RCC), and non-coronary cusp (NCC).
- The coronary arteries originate from the left and right aortic sinuses.
2. Blood Supply to the Heart
Arterial Supply
- The heart’s arterial blood supply comes from the right and left coronary arteries, the first branches of the aorta.
- Left Coronary Artery divides into:
- Anterior interventricular artery: Supplies the interventricular septum and anterior walls of both ventricles.
- Circumflex artery: Supplies the left atrium and posterior walls of the left ventricle.
- Right Coronary Artery branches into:
- Right marginal artery: Supplies the right lateral side of the myocardium.
- Posterior interventricular artery: Supplies the posterior ventricular walls.
- Left Coronary Artery divides into:
Venous Drainage
- The heart’s venous blood is drained by coronary veins into the coronary sinus, which empties into the right atrium. Major tributaries:
- Great cardiac vein: Drains areas supplied by the left coronary artery.
- Middle cardiac vein: Drains areas supplied by the posterior interventricular artery.
- Small cardiac vein: Drains the right atrium and ventricle.
3. Nerve Supply to the Heart
Sympathetic Nerve Actions
- Sympathetic innervation originates from thoracic segments (T1–T4) of the spinal cord.
- These fibers synapse in cervical and thoracic ganglia and extend to the cardiac plexus.
- Sympathetic stimulation increases heart rate and contractility, and constricts coronary vessels.
Parasympathetic Nerve Actions
- Parasympathetic fibers are supplied by the vagus nerve (CN X).
- These fibers decrease heart rate, reduce the force of contraction, and dilate coronary vessels, especially affecting the sinoatrial node (SA node).
Higher Centers
- The medulla oblongata is the primary control center for autonomic regulation, with input from the hypothalamus, which adjusts the cardiovascular response based on stress, emotion, and temperature.
4. Cardiac Muscle Fibers
Structure of Cardiac Muscle Fibers
- Cardiac muscle fibers are shorter and less circular than skeletal muscle fibers, creating a "stair-step" appearance due to branching.
- Each fiber is 50–100 μm long with a diameter of 14 μm. The fibers have a centrally located nucleus.
Intercalated Discs
- The cardiac muscle fibers are connected by intercalated discs, which feature:
- Desmosomes: Anchor the fibers together, ensuring the cells do not pull apart during contraction.
- Gap junctions: Allow electrical impulses to propagate quickly between cells, ensuring coordinated contraction of the myocardium.
Functional Arrangement
- Cardiac fibers are arranged in a spiral or circular manner, allowing for efficient pumping actions.
Blood Vessels:
Blood Volume
- The average adult male has approximately 5-6 liters of blood. This blood circulates through the body via various types of blood vessels.
Types of Blood Vessels
- Arteries:
- Function: Transport oxygenated blood from the heart to the tissues.
- Exception: The pulmonary artery carries deoxygenated blood from the heart to the lungs.
- Capillaries:
- Microscopic vessels responsible for exchanging gases, nutrients, and waste between blood and tissues.
- Return deoxygenated blood to the veins.
- Veins:
- Function: Return deoxygenated blood to the heart.
- Exception: Pulmonary veins carry oxygenated blood from the lungs to the heart.
Structure of Blood Vessels
- Tunica Externa (Adventitia):
- Outermost layer composed of loose connective tissue.
- Provides support, protection, and prevents overstretching.
- Tunica Media:
- Middle layer made of smooth muscle.
- Involved in regulating blood vessel diameter through constriction and dilation.
- Tunica Interna (Intima):
- Innermost layer, consisting of endothelial cells.
- Creates a smooth lining for blood flow.
Blood Flow Pathway
- Blood flows from the heart through the following structures:
- Aorta
- Arteries
- Arterioles
- Capillaries
- Venules
- Veins
- Superior/Inferior Vena Cava
- Blood returns to the heart via the vena cava.
The Arterial System
- The arterial system carries oxygenated blood from the heart to the capillaries.
- Four main types of arteries exist, each with distinct structures and functions:
Major Arterial Supply
- Aorta and its branches
- Neck and head arterial supply
- Upper extremities
- Thorax
- Abdomen
- Pelvic region and lower extremities
Types of Arteries
-
Elastic Arteries:
- Function: Conduct blood from the heart to distant regions of the body.
- Structure:
- Tunica Intima: Endothelium and connective tissue with elastic laminae.
- Tunica Media: Thickest layer, comprising 40-70 fenestrated elastic membranes with smooth muscle and collagen.
- Tunica Adventitia: Thin, contains lymphatics, nerves, and vasa vasorum (small blood vessels that supply the larger vessel walls).
-
Muscular Arteries:
- Medium-sized arteries, responsible for distributing blood to organs and tissues.
- Structure:
- Tunica Intima: Endothelium with a thick elastic lamina.
- Tunica Media: About 40 layers of smooth muscle, connected via gap junctions for coordinated contraction.
- Tunica Adventitia: Contains vasa vasorum, lymphatics, and nerve fibers.
-
Arterioles:
- Function: Part of the microcirculation, transporting blood from muscular arteries to metarterioles.
- Structure:
- Arterioles are classified as having a diameter of less than 0.1 mm.
- Around 3 layers of smooth muscle, with the internal elastic lamina absent.
- The external elastic lamina is only present in larger arterioles.
-
Metarterioles:
- Supply blood to capillary beds.
- Structure: Instead of continuous smooth muscle, they have rings of muscle (precapillary sphincters) at certain points that regulate blood flow into capillaries.
The Capillaries
- Capillaries consist of a single layer of endothelium, allowing efficient diffusion of gases and nutrients.
- Capillaries function as part of capillary beds, networks of interwoven capillaries.
Types of Capillaries:
-
Continuous Capillaries:
- Characterized by uninterrupted endothelial linings.
- Function: Permit passage of small molecules like water and ions.
- Examples: Found in skeletal muscles, skin, and the gonads.
-
Fenestrated Capillaries:
- Have pores in their endothelial cells.
- Function: Permit larger molecules to pass through.
- Examples: Found in endocrine glands, intestines, and kidneys.
-
Sinusoidal Capillaries:
- Larger and more irregularly shaped, with gaps between endothelial cells.
- Function: Allow the passage of cells and large molecules.
- Examples: Found in bone marrow, lymph nodes, and adrenal glands.
The Venous System
The venous system is responsible for returning deoxygenated blood from the body’s tissues back to the heart. The key components of the venous system include venules, veins, and major venous drainages. With the exception of the pulmonary veins, which carry oxygenated blood from the lungs to the heart, the venous system primarily handles deoxygenated blood.
Major Venous Drainages
-
Venous Drainage of the Head and Neck:
- Blood from the head and neck is primarily drained by the jugular veins (internal and external).
- The internal jugular vein collects blood from the brain, while the external jugular vein drains blood from the superficial areas of the head and neck.
-
Major Tributaries of the Inferior Vena Cava:
- The inferior vena cava is the largest vein in the body, returning blood from the lower half of the body to the right atrium of the heart.
- Major tributaries include the hepatic veins (from the liver), renal veins (from the kidneys), and common iliac veins (from the pelvis and lower limbs).
-
Venous Drainage of the Upper Extremities:
- Blood from the upper limbs is drained by the subclavian veins.
- The superficial veins, such as the cephalic vein and basilic vein, play a significant role in this drainage.
-
Venous Drainage of the Lower Extremities:
- Blood from the lower limbs is drained by both superficial and deep veins, including the femoral vein and great saphenous vein.
Post-Capillary Venules
Post-capillary venules are the smallest vessels in the venous system and are responsible for collecting blood from capillary beds. Their structure is simple but vital:
- Endothelial lining: Forms the wall of the post-capillary venules.
- Pericytes: Support the endothelial cells, contributing to the integrity and function of the vessel.
- Diameter: These vessels are 10-30 micrometers in diameter.
Venules
Venules are larger than post-capillary venules and are responsible for transporting blood away from the capillary beds to larger veins. Their structure includes:
- Endothelium with pericytes: These cells support the thin walls of the venules.
- Valves: Venules contain valves to prevent the backflow of blood, ensuring unidirectional flow towards the heart.
- Diameter: Venules can reach up to 1mm in diameter.
Veins
Veins are the largest vessels in the venous system, acting as the final pathway for blood to return to the heart. Their structure differs from arteries in several key ways:
- Larger diameter and thinner wall: Veins have larger lumens compared to arteries, but their walls are thinner, with less muscle and elastic tissue.
- Valves: Veins contain valves to prevent the backflow of blood, which, in conjunction with skeletal muscle contractions, helps push blood toward the heart.
Classification by Size:
-
Small and Medium Veins:
- They have a well-developed tunica adventitia (outer layer) and thin tunica intima (inner layer) and tunica media (middle layer).
- They have a well-developed tunica adventitia (outer layer) and thin tunica intima (inner layer) and tunica media (middle layer).
-
Large Veins:
- Large veins (diameter > 10mm) have thicker tunica intima and a well-developed smooth muscle layer in the tunica adventitia.
- Large veins (diameter > 10mm) have thicker tunica intima and a well-developed smooth muscle layer in the tunica adventitia.
The Great Arteries
The aorta is the largest artery in the body and plays a central role in systemic circulation, transporting oxygenated blood from the heart to the rest of the body. The aorta can be divided into four sections:
-
Ascending Aorta:
- Arises from the left ventricle and is 2 inches long.
- Branches: Includes the right and left coronary arteries, which supply the heart muscle with oxygenated blood.
-
Aortic Arch:
- Continuation of the ascending aorta, arches superiorly and posteriorly, and ends at the T4 vertebra.
- Branches:
- Brachiocephalic trunk (divides into the right common carotid and right subclavian arteries).
- Left common carotid artery (supplies the left side of the head and neck).
- Left subclavian artery (supplies the left upper limb).
-
Thoracic Aorta:
- The thoracic aorta (T4-T12 vertebrae) descends through the chest and becomes the abdominal aorta after passing through the diaphragm.
- Branches: Includes the bronchial, mediastinal, esophageal, pericardial, superior phrenic, intercostal, and subcostal arteries.
-
Abdominal Aorta:
- Extends from T12 to L4, where it bifurcates into the right and left common iliac arteries.
- Branches:
- Inferior Phrenic Arteries (T12): Supply the diaphragm.
- Superior Mesenteric Artery (L1): Supplies the intestines.
- Coeliac Artery (T12): Supplies the liver, stomach, spleen, and pancreas.
- Middle Suprarenal Arteries (L1): Supply the adrenal glands.
- Renal Arteries (L1-L2): Supply the kidneys.
- Gonadal Arteries (L2): Supply the testes in males and ovaries in females.
- Inferior Mesenteric Artery (L3): Supplies the large intestine and rectum.
- Median Sacral Artery (L4): Supplies the coccyx and sacrum.
- Lumbar Arteries: Supply the abdominal wall and spinal cord.
- Common Iliac Arteries: Terminal branches of the abdominal aorta supplying the pelvis and lower limbs.
Common Iliac Arteries:
- External Iliac Artery: Continues as the femoral artery in the lower limb.
- Internal Iliac Artery: Supplies the pelvic organs.
The Venous System
1. Superior Vena Cava
The superior vena cava (SVC) is a large vein that carries deoxygenated blood from the body’s upper regions to the heart. It drains blood from the head, neck, upper limbs, and chest.
- Major Branches:
- Right brachiocephalic vein and left brachiocephalic vein: These veins are formed by the union of the internal jugular veins and subclavian veins. The brachiocephalic veins merge to form the superior vena cava, which delivers blood to the right atrium.
2. Inferior Vena Cava
The inferior vena cava (IVC) is the largest vein in the body, responsible for returning deoxygenated blood from the regions below the diaphragm.
- Formation: The IVC is formed at the level of the L5 vertebra by the joining of the right and left common iliac veins.
- Venous Tributaries:
- Receives blood from the abdominal walls, gonads, kidneys, and other structures.
- Ends as it enters the right atrium of the heart through the inferior aspect.
Veins of the Head and Neck
The head and neck are drained primarily by three paired veins:
- External Jugular Veins: These veins drain superficial structures of the scalp and face and empty into the subclavian veins.
- Internal Jugular Veins: These veins are the main venous drainage for the brain, collecting blood from the dural venous sinuses and emptying into the brachiocephalic veins after joining with the subclavian veins.
- Vertebral Veins: Drain the cervical vertebrae, spinal cord, and small neck muscles. They run through the transverse foramina of the cervical vertebrae and empty into the brachiocephalic veins.
Dural Venous Sinuses
The dural venous sinuses are channels found between the layers of the dura mater in the brain. These sinuses collect blood from the brain and direct it toward the internal jugular veins.
- Inferior sagittal sinus drains into the straight sinus.
- Both the superior sagittal sinus and the straight sinus drain into the transverse sinuses, which flow into the sigmoid sinuses and eventually into the internal jugular veins.
- Cavernous sinuses receive blood from the ophthalmic veins and facial veins (nose and upper lip area).
Veins of the Upper Limbs and Thorax
-
Superficial Veins:
- These veins are larger than their deep counterparts and include the cephalic vein and basilic vein, which drain into the axillary vein.
- The median cubital vein, located in the forearm, is a common site for blood draws.
-
Deep Veins:
- The radial and ulnar veins unite to form the brachial vein.
- The brachial vein becomes the axillary vein, and then the subclavian vein at the level of the first rib.
The Azygos System
The azygos system is a network of veins that drain the thoracic wall and thoracic organs.
-
Azygos Vein: Runs along the right side of the vertebral column, receiving blood from the right posterior intercostal veins and right ascending lumbar vein. It arches at the level of T4 to empty into the superior vena cava.
-
Hemiazygos Vein: Ascends on the left side of the vertebral column and drains the lower left thoracic wall.
-
Accessory Hemiazygos Vein: Drains the middle thorax and empties into the azygos vein.
Veins of the Abdomen
- Lumbar Veins: Drain the posterior abdominal wall and empty into both the inferior vena cava and the ascending lumbar veins.
- Gonadal Veins:
- The right gonadal vein drains into the IVC.
- The left gonadal vein drains into the left renal vein.
- Renal Veins: These veins drain blood from the kidneys directly into the IVC.
- Suprarenal Veins:
- The right suprarenal vein drains into the IVC, while the left suprarenal vein drains into the left renal vein.
Portal Circulation
The hepatic portal system is a vital circulation pathway that collects nutrient-rich blood from the digestive organs and delivers it to the liver.
- Hepatic Portal Vein: Formed by the convergence of the superior mesenteric vein and splenic vein.
- Superior Mesenteric Vein: Drains the small intestine, part of the large intestine, and the stomach.
- Splenic Vein: Drains the spleen, parts of the stomach, and pancreas.
- Inferior Mesenteric Vein: Drains the distal portion of the large intestine and rectum, joining the splenic vein.
Veins of the Lower Limbs
- Deep Veins:
- The posterior tibial vein receives blood from the fibular vein and joins the anterior tibial vein to form the popliteal vein.
- The popliteal vein becomes the femoral vein, which eventually transitions into the external iliac vein in the pelvis.
- Superficial Veins:
- The great saphenous vein and small saphenous vein arise from the dorsal venous arch of the foot.
Fetal Circulation
In the fetus, special structures allow blood to bypass non-functional organs like the lungs and liver.
- Umbilical Arteries: Carry deoxygenated blood from the fetus to the placenta.
- Umbilical Vein: Returns oxygenated blood from the placenta to the fetus.
- Ductus Venosus: Shunts blood from the umbilical vein, bypassing the liver.
- Foramen Ovale: A hole in the atrial septum that allows blood to bypass the lungs by flowing from the right atrium to the left atrium.
- Ductus Arteriosus: Connects the pulmonary artery to the aorta, allowing blood to bypass the lungs.
Blood and its Components
Blood is a vital fluid circulating in the body, composed of plasma and various types of cells. It performs essential functions in the body, including transporting oxygen, nutrients, and hormones, protecting the body against diseases, and helping regulate temperature.
Functions of Blood
- Nutrient Supply: Delivers glucose, fatty acids, and amino acids to cells.
- Gas Transport: Transports oxygen (O₂) from the lungs to tissues and carbon dioxide (CO₂) back to the lungs for exhalation.
- Protection: Contains white blood cells that fight off pathogens, and platelets that prevent blood loss during injuries.
- Regulation: Helps maintain body temperature and homeostasis.
Physical Characteristics
- Blood is more viscous than water.
- Normal temperature: 100.4°F.
- Blood makes up about 8% of body weight.
- Blood volume:
- Males: 5-6 liters.
- Females: 4-5 liters.
Components of Blood
Blood consists of two major components:
- Blood Cells (45%)
- Plasma (55%)
Blood Cells
There are three main types of blood cells:
-
Red Blood Cells (RBCs):
- Structure: Biconcave shape, elastic membrane, and no nucleus. 95% of the RBC's structure consists of hemoglobin.
- Function: Transport oxygen and carbon dioxide.
- Life Span: About 4 months.
- Formation: Occurs in red bone marrow.
- Count: Males have around 5-5.5 million RBCs/mm³, while females have 4-4.5 million RBCs/mm³.
-
White Blood Cells (WBCs):
- Structure: Colorless and larger than RBCs.
- Function: Key role in the immune system, defending against infection.
- Life Span: Can last from a few days to years, depending on the body's needs.
- Types:
- Granulocytes: Neutrophils, eosinophils, and basophils (contain granules).
- Agranulocytes: Monocytes and lymphocytes (lack granules).
- Count: 7,000-8,000 WBCs/mm³ in healthy individuals.
-
Platelets:
- Structure: Small fragments of larger cells (megakaryocytes) with no nucleus.
- Function: Facilitate blood clotting (hemostasis) to prevent excessive blood loss.
- Life Span: 5-9 days.
- Count: 150,000-400,000 platelets/drop of blood.
Plasma
- Plasma makes up 55% of blood and is about 90% water.
- Contents: Plasma contains proteins, inorganic ions (salts), nutrients, waste products, hormones, and gases.
Functions of Plasma:
- Helps maintain blood pressure.
- Regulates body temperature.
- Carries essential minerals and nutrients that play important roles in body functions.
Disorders of Blood
-
Anemia:
- Characterized by a deficiency of RBCs, leading to reduced oxygen-carrying capacity.
- Symptoms: Fatigue, cold intolerance, pale skin.
- Cause: Lack of RBCs means less oxygen for energy (ATP) production.
-
Leukemia:
- Cancer characterized by uncontrolled production of WBCs.
- Symptoms: Tiredness, fever, weight loss, pale skin.
- Treatment: Regular blood transfusions and bone marrow transplants.
-
Thalassemia:
- A genetic disorder where abnormal hemoglobin production affects RBCs.
- Common in children of Mediterranean descent.
- Treatment: Regular blood transfusions and bone marrow transplant.


Free Videos