Physiology Of Respiratory System
The Respiratory System
The respiratory system is a network of organs and tissues that help in breathing, exchanging gases such as oxygen (O2) and carbon dioxide (CO2) between the body and the environment. The major components include:
- Nasal Cavity
- Pharynx
- Larynx
- Trachea
- Bronchi
- Lungs
Together, these organs form the Respiratory Tract, which can be divided into:
- Upper Respiratory Tract: Nasal cavity, pharynx, and associated structures.
- Lower Respiratory Tract: Larynx, trachea, bronchi, and lungs.
2. Structure of the Lungs and Alveoli
The lungs are the primary organs of respiration and are subdivided into smaller units called alveoli, where gas exchange occurs. Each human lung contains around 700 million alveoli, which provide a large surface area (approximately 145 square meters) crucial for the exchange of O2 and CO2 with surrounding blood capillaries.
2.1 Respiratory Unit
The terminal portion of the respiratory tract is the respiratory unit, which includes:
- Respiratory Bronchioles
- Alveolar Ducts
- Antrum
- Alveolar Sacs
- Alveoli
3. Microscopic Structure of Alveoli
The alveoli are lined by a single layer of epithelial cells and are surrounded by capillaries. They are the site where the actual exchange of gases takes place, facilitated by the thin alveolar membrane and large surface area.
4. Types of Respiration
There are two types of respiration:
- External Respiration: The exchange of O2 and CO2 between the lungs and blood.
- Internal Respiration: The exchange of gases between the blood and tissues.
5. Functions of the Respiratory System
5.1 Respiratory Functions
- Pulmonary Ventilation: The process of moving air in and out of the lungs (breathing).
- Diffusion of O2 and CO2: Gas exchange between alveoli and the blood.
- Transportation of O2 and CO2: Transport of gases in the blood to and from body tissues.
- Regulation of Ventilation: The body controls the rate and depth of breathing based on its needs.
5.2 Non-Respiratory Functions
- Olfaction: The sense of smell.
- Vocalization: Production of sounds, involving the larynx.
- Defense Mechanisms: Protection against pathogens via mucus and cilia.
- Anticoagulant Function: Producing anticoagulants to prevent blood clotting.
- Regulation of Body Temperature and Acid-Base Balance: Helps maintain homeostasis.
- Water Balance: Maintains moisture in the respiratory tract.
- Secretion of Angiotensin-Converting Enzyme (ACE): Plays a role in blood pressure regulation.
6. Mechanism of Respiration
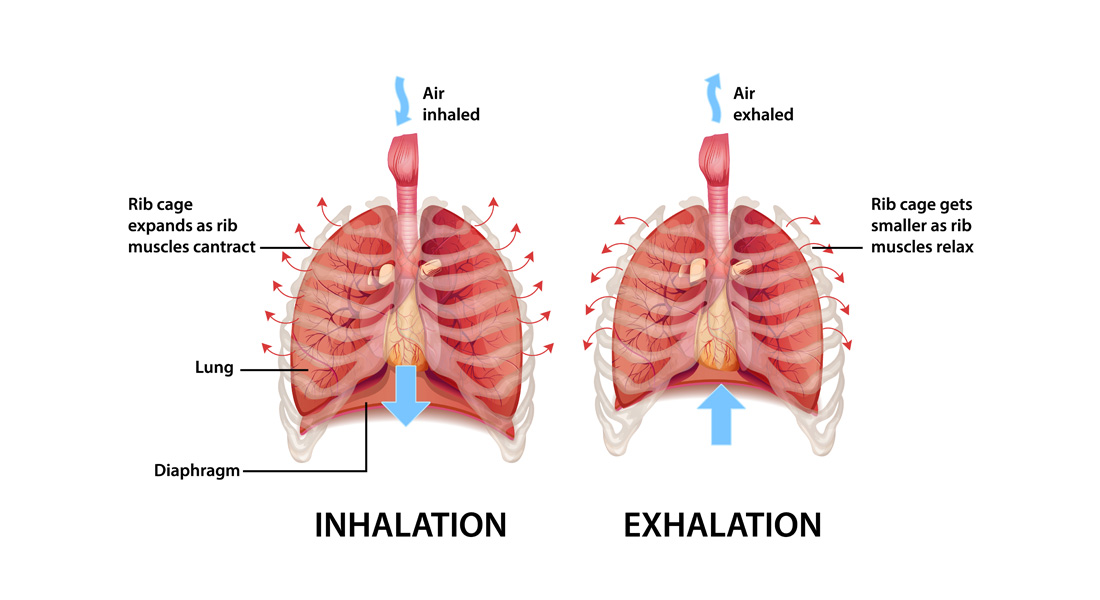
Breathing involves coordinated muscle movements that expand and contract the thoracic cavity.
6.1 Muscles of Respiration
- Primary Inspiratory Muscles: Diaphragm (main muscle responsible for breathing).
- Accessory Inspiratory Muscles: Sternomastoid, scaleni, pectorals, etc., used during deep or forced inspiration.
- Primary Expiratory Muscles: Internal intercostal muscles.
- Accessory Expiratory Muscles: Abdominal muscles used during forced expiration.
6.2 Inspiration
- Diaphragm contraction increases the thoracic cavity's superior-inferior dimension.
- External intercostal muscle contraction expands the lateral and anterior-posterior dimensions of the ribcage.
- This expansion leads to a decrease in pulmonary pressure (by 1 mm Hg), allowing air to rush into the lungs and fill the alveoli.
6.3 Expiration
- Quiet Expiration: A passive process where the lungs' natural elasticity reduces their volume, increasing pulmonary pressure and forcing air out.
- Forced Expiration: Involves contraction of the abdominal muscles to reduce lung volume further, increasing pressure and expelling more air.
7. Pulmonary Volumes and Capacities
Respiratory volumes measure the amount of air involved in breathing, while capacities combine these volumes to give a fuller picture of lung function.
7.1 Pulmonary Volumes
- Tidal Volume (TV): The normal volume of air moved in and out during breathing (~0.5 L).
- Inspiratory Reserve Volume (IRV): Additional air inhaled after normal tidal volume (~2.1-3.2 L).
- Expiratory Reserve Volume (ERV): Additional air exhaled after normal tidal volume (~1-2 L).
- Residual Volume (RV): Air remaining in the lungs after forced exhalation (~1.2 L).
7.2 Respiratory Capacities
- Inspiratory Capacity (IC): TV + IRV (the maximum volume of air that can be inhaled).
- Functional Residual Capacity (FRC): ERV + RV (the volume of air left in the lungs after normal exhalation).
- Vital Capacity (VC): TV + IRV + ERV (the total volume of air that can be exhaled after maximal inhalation).
- Total Lung Capacity (TLC): TV + IRV + ERV + RV (~6 L), the sum of all lung volumes.
7.3 Dead Space
- Anatomical Dead Space: All areas of the respiratory tract where gas exchange does not occur.
- Alveolar Dead Space: Non-functional alveoli.
- Total Dead Space: Anatomical + Alveolar.
8. Pulmonary Function Tests
- Spirometer: Measures respiratory volumes and capacities to assess lung function.
- Obstructive Pulmonary Disease: Characterized by increased airway resistance (e.g., bronchitis or asthma).
- Restrictive Disorders: Marked by decreased lung capacity (e.g., tuberculosis or polio).
9. Transport of Gases
Oxygen and carbon dioxide are transported through the bloodstream by:
- Oxygen (O2): 3% dissolved in plasma, 97% bound to hemoglobin (Hb).
- Carbon Dioxide (CO2): Transported as dissolved gas (7%), bicarbonate (63%), and carbamino compounds (30%).
9.1 Oxygen-Hemoglobin Dissociation Curve
- 104 mmHg in the lungs results in 100% hemoglobin saturation.
- 40 mmHg in tissues results in 75% saturation.
- Right Shift: Reduced affinity for oxygen, more unloading (e.g., due to increased temperature or lower pH).
- Left Shift: Increased affinity for oxygen, less unloading (e.g., due to lower temperature or higher pH).
9.2 Carbon Dioxide Dissociation Curve
CO2 forms bicarbonate through the Bohr Effect, where decreased pH (increased H+ concentration) promotes O2 unloading in tissues.
10. Applied Aspects of Respiratory Disorders
- Lung Cancer: Includes small cell and non-small cell lung cancers. Symptoms include chronic cough, chest pain, and difficulty breathing.
- Chronic Obstructive Pulmonary Disease (COPD): Includes asthma, chronic bronchitis, and emphysema, characterized by obstruction of airflow and breathing difficulties.
- Pulmonary Embolism: A blockage in the pulmonary artery, usually due to a blood clot.
- Cystic Fibrosis: A genetic disorder causing thick mucus production, leading to lung and digestive system issues.
- Pneumonia: Infection of the lungs leading to fluid accumulation, with types including lobar and bronchial pneumonia.
- Tuberculosis: A bacterial infection primarily affecting the lungs, causing chronic cough, weight loss, and fatigue.


Free Videos