The Cardiovascular System
The Cardiovascular System comprises the heart and an extensive network of blood vessels that circulate blood throughout the body. This system is essential for sustaining life by performing several critical functions.
Functions of the Cardiovascular System
-
Circulates Oxygen and Removes Carbon Dioxide
- Delivers oxygen from the lungs to body tissues.
- Removes carbon dioxide, a metabolic waste product, from tissues to the lungs for exhalation.
-
Provides Cells with Nutrients
- Transports essential nutrients (glucose, amino acids, fatty acids) from the digestive system to cells.
- Transports essential nutrients (glucose, amino acids, fatty acids) from the digestive system to cells.
-
Removes Waste Products
- Carries metabolic wastes (urea, creatinine) to excretory organs (kidneys, liver) for disposal.
- Carries metabolic wastes (urea, creatinine) to excretory organs (kidneys, liver) for disposal.
-
Transports Hormones
- Delivers hormones from endocrine glands to target cells and organs, facilitating communication and regulation of bodily functions.
- Delivers hormones from endocrine glands to target cells and organs, facilitating communication and regulation of bodily functions.
-
Regulates Body Temperature
- Distributes heat produced by metabolic activities, helping maintain a stable internal body temperature.
- Distributes heat produced by metabolic activities, helping maintain a stable internal body temperature.
Components of the Cardiovascular System
The cardiovascular system consists of three primary functional components:
- Heart
- Blood Vessels
- Blood
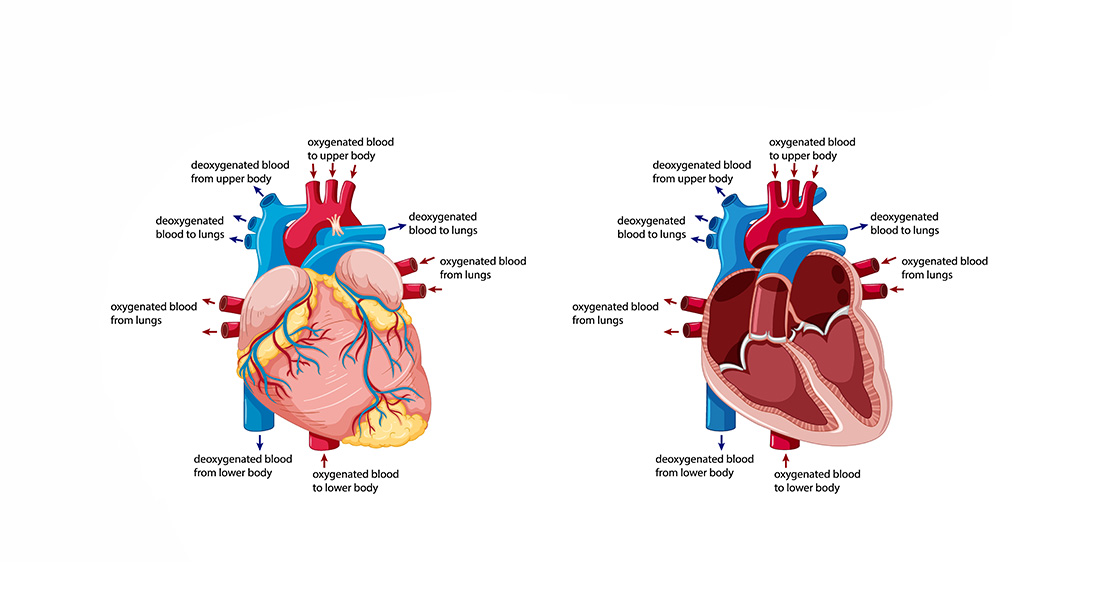
Pathways of Blood Flow
Blood circulates through two main pathways originating from the heart:
-
Pulmonary Circulation
- Route: Heart → Lungs → Heart
- Function: Oxygenates blood by removing carbon dioxide and adding oxygen.
-
Systemic Circulation
- Route: Heart → Body Tissues → Heart
- Function: Delivers oxygenated blood to tissues and returns deoxygenated blood to the heart.
Pulmonary Circulation
Overview
Pulmonary circulation is a short loop that transports blood between the heart and the lungs.
Key Components
-
Pulmonary Artery
- Origin: Left ventricle of the heart.
- Function: Carries deoxygenated blood from the heart to the lungs.
- Exception: Unlike other arteries, it carries deoxygenated blood.
-
Lungs
- Function: Gas exchange occurs here. Blood picks up oxygen and releases carbon dioxide.
- Function: Gas exchange occurs here. Blood picks up oxygen and releases carbon dioxide.
-
Pulmonary Veins
- Function: Return oxygenated blood from the lungs to the heart.
- Exception: Unlike other veins, they carry oxygenated blood.
Blood Flow in Pulmonary Circulation
- Left Ventricle → Pulmonary Artery → Lungs
- Lungs → Pulmonary Veins → Left Atrium → Left Ventricle
Systemic Circulation
Overview
Systemic circulation is a comprehensive loop that transports blood between the heart and the rest of the body.
Key Components
-
Left Ventricle
- Function: Pumps oxygenated blood into the aorta for distribution to the body.
- Function: Pumps oxygenated blood into the aorta for distribution to the body.
-
Aorta and Arterial System
- Function: Distributes oxygenated blood to various tissues via arteries and arterioles.
- Function: Distributes oxygenated blood to various tissues via arteries and arterioles.
-
Capillaries
- Function: Site of exchange of nutrients, gases, and waste products between blood and tissues.
- Function: Site of exchange of nutrients, gases, and waste products between blood and tissues.
-
Venous System
- Function: Collects deoxygenated blood from tissues and returns it to the heart via veins and venules.
- Function: Collects deoxygenated blood from tissues and returns it to the heart via veins and venules.
-
Right Atrium
- Function: Receives deoxygenated blood from systemic circulation.
- Function: Receives deoxygenated blood from systemic circulation.
-
Right Ventricle
- Function: Pumps deoxygenated blood into the pulmonary circulation via the pulmonary artery.
- Function: Pumps deoxygenated blood into the pulmonary circulation via the pulmonary artery.
Blood Flow in Systemic Circulation
- Left Ventricle → Aorta → Arteries → Arterioles → Capillaries → Venules → Veins → Superior/Inferior Vena Cava → Right Atrium → Right Ventricle → Pulmonary Artery
Functional Anatomy of the Heart
General Description
- Location: Centrally situated within the thoracic cavity, lying beneath the sternum and between the lungs.
- Enclosure: Surrounded by the pericardium, a double-walled fibrous sac that anchors the heart and reduces friction during heartbeats.
- Size: Approximately the size of a closed fist.
Structure of the Heart
-
Layers of the Heart Wall
- Epicardium: Outermost layer; a thin membrane covering the heart's external surface.
- Myocardium: Middle muscular layer; responsible for the heart's contractile force.
- Endocardium: Innermost layer; lines the heart chambers and valves, continuous with the endothelium of blood vessels.
-
Chambers of the Heart
- Atria (2)
- Right Atrium: Receives deoxygenated blood from systemic circulation.
- Left Atrium: Receives oxygenated blood from pulmonary circulation.
- Ventricles (2)
- Right Ventricle: Pumps deoxygenated blood to the lungs via the pulmonary artery.
- Left Ventricle: Pumps oxygenated blood to the body via the aorta.
- Septum: Muscular wall separating the left and right sides of the heart.
- Atria (2)
-
Valves of the Heart
- Atrioventricular (AV) Valves
- Tricuspid Valve: Between the right atrium and right ventricle; has three cusps.
- Mitral (Bicuspid) Valve: Between the left atrium and left ventricle; has two cusps.
- Semilunar Valves
- Pulmonary Valve: Between the right ventricle and pulmonary artery; prevents backflow into the ventricle.
- Aortic Valve: Between the left ventricle and aorta; prevents backflow into the ventricle.
- Function: Maintain unidirectional blood flow through the heart chambers and into the arteries.
- Atrioventricular (AV) Valves
Properties of Myocardium
The myocardium is the muscular tissue of the heart, essential for its pumping action. It possesses unique properties that enable efficient and coordinated contractions.
Characteristics of Cardiac Muscle
- Striated: Exhibits a striped appearance due to the arrangement of actin and myosin filaments.
- Short, Branched Cells: Facilitate electrical connectivity and synchronized contractions.
- Uninucleate: Typically contains a single nucleus per cell.
- Intercalated Discs: Specialized connections between cardiac cells that facilitate rapid electrical communication and mechanical linkage.
Functional Specializations of Myocardial Cells
-
Automaticity
- Ability to generate spontaneous action potentials without external stimuli.
- Pacemaker Cells: Located in the sinoatrial (SA) node, atrioventricular (AV) node, and Purkinje fibers.
- SA Node: Primary pacemaker with an intrinsic rate of 60-100 beats/min.
- AV Node: Secondary pacemaker with an intrinsic rate of 40-60 beats/min.
- Purkinje Fibers: Tertiary pacemaker with an intrinsic rate of ~35 beats/min.
-
Excitability
- Ability to respond to stimuli by generating action potentials.
- Action Potential Phases in Contractile Cells:
- Phase 0 (Depolarization): Rapid influx of Na⁺ ions via voltage-gated channels.
- Phase 1 (Initial Repolarization): Transient K⁺ efflux causing a slight repolarization.
- Phase 2 (Plateau Phase): Balance between Ca²⁺ influx and K⁺ efflux.
- Phase 3 (Repolarization): Closure of Ca²⁺ channels and increased K⁺ efflux leading to repolarization.
- Phase 4 (Resting Membrane Potential): Stable negative membrane potential maintained by ion pumps.
-
Conduction
- Rapid transmission of electrical impulses through the heart to ensure coordinated contractions.
- Intrinsic Conduction System: Includes SA node, AV node, Bundle of His, bundle branches, and Purkinje fibers.
-
Contraction
- Mechanism by which myocardial cells generate force to pump blood.
- Excitation-Contraction Coupling:
- Action potential spreads across the sarcolemma and into T-tubules.
- Ca²⁺ influx triggers further Ca²⁺ release from the sarcoplasmic reticulum.
- Ca²⁺ binds to troponin, facilitating actin-myosin interactions and muscle contraction.
Contractile vs. Autorhythmic Cells
- Contractile Cells
- Responsible for the mechanical contraction of the heart.
- Features:
- Numerous mitochondria for energy.
- Well-developed sarcoplasmic reticulum.
- Organized sarcomere structure for efficient contraction.
- Autorhythmic (Pacemaker) Cells
- Responsible for initiating and regulating the heartbeat.
- Features:
- Smaller size with fewer myofibrils.
- Unstable membrane potential allowing spontaneous depolarization.
- Lack organized sarcomere structure; do not contribute to contractile force.
Cardiac Cycle
The Cardiac Cycle encompasses all events associated with blood flow through the heart during one complete heartbeat. It is divided into two primary phases: Systole (contraction) and Diastole (relaxation).
Phases of the Cardiac Cycle
-
Ventricular Systole (0.33 sec)
- Isovolumic Contraction (0.08 sec)
- Phase 1: Asynchronous Contraction (0.05 sec)
- Onset of ventricular contraction.
- AV valves close to prevent backflow into atria.
- SL (semilunar) valves remain closed.
- Ventricular volume remains constant; pressure rises.
- Phase 2: Isovolumic Contraction (0.03 sec)
- Rapid increase in ventricular pressure.
- SL valves remain closed.
- Ventricular volume remains unchanged.
- Phase 1: Asynchronous Contraction (0.05 sec)
- Ejection Phase (0.25 sec)
- Phase 3: Rapid Ejection (0.12 sec)
- Ventricular pressure exceeds arterial pressure.
- SL valves open; blood is ejected rapidly.
- Ventricular volume decreases significantly.
- Phase 4: Reduced Ejection (0.13 sec)
- Ventricular pressure continues to drop.
- Ejection rate slows.
- Ventricular volume continues to decrease but at a slower rate.
- Phase 3: Rapid Ejection (0.12 sec)
- Isovolumic Contraction (0.08 sec)
-
Ventricular Diastole (0.47 sec)
- Isovolumic Relaxation (0.12 sec)
- Phase 5: Protodiastole (0.04 sec)
- Ventricles begin to relax.
- SL valves close to prevent backflow.
- AV valves remain closed.
- Ventricular volume remains constant.
- Phase 6: Isovolumic Relaxation (0.08 sec)
- Ventricular pressure drops rapidly.
- All valves remain closed.
- Ventricular volume remains unchanged.
- Phase 5: Protodiastole (0.04 sec)
- Filling Phase (0.35 sec)
- Phase 7: Rapid Filling (0.08 sec)
- AV valves open as ventricular pressure falls below atrial pressure.
- Blood flows rapidly from atria to ventricles.
- Ventricular volume increases sharply.
- Phase 8: Reduced Filling (0.17 sec)
- Filling rate slows as ventricular pressure approaches atrial pressure.
- Ventricular volume continues to increase at a slower rate.
- Phase 7: Rapid Filling (0.08 sec)
- Presystole (0.1 sec)
- Phase 9: Presystole (0.1 sec)
- Atrial contraction (atrial systole) tops off ventricular filling.
- Ventricular volume increases slightly.
- Prepares the heart for the next cycle of systole.
- Phase 9: Presystole (0.1 sec)
- Isovolumic Relaxation (0.12 sec)
Summary of Cardiac Cycle Phases
-
Ventricular Systole
- Contraction of ventricles.
- Ejection of blood into pulmonary and systemic circulations.
-
Ventricular Diastole
- Relaxation of ventricles.
- Filling of ventricles with blood from atria.
Visualization of Cardiac Cycle
A ventricular systole followed by a ventricular diastole constitutes one complete cardiac cycle, typically lasting about 0.8 seconds (for a heart rate of 75 beats per minute).
Cardiac Output
Cardiac Output (CO) is the volume of blood pumped by the left ventricle per minute. It is a critical indicator of heart function and overall cardiovascular health.
Calculation of Cardiac Output
Cardiac Output (CO)=Stroke Volume (SV)×Heart Rate (HR)
-
Stroke Volume (SV): Volume of blood ejected with each heartbeat.
SV = End-Diastolic Volume (EDV) − End-Systolic Volume (ESV)
Ex: SV = 135mL−65mL = 70mL -
Heart Rate (HR): Number of heartbeats per minute.
HR=72 beats/mi
Factors Influencing Cardiac Output
-
Heart Rate (HR)
- Increased by sympathetic stimulation, exercise, stress.
- Decreased by parasympathetic stimulation, rest.
-
Stroke Volume (SV)
- Preload: Degree of ventricular filling; increased preload raises SV.
- Afterload: Resistance against ventricular ejection; increased afterload can decrease SV.
- Contractility: Intrinsic ability of the heart muscle to contract; increased contractility raises SV.
Blood Pressure
Blood Pressure (BP) is the force exerted by circulating blood on the walls of blood vessels. It is a vital sign indicating the force and rate of blood flow.
Components of Blood Pressure
-
Systolic Pressure
- Definition: Pressure in the arteries during ventricular contraction.
- Typical Value: ~120 mm Hg
- Significance: Indicates the force when the heart pumps blood.
-
Diastolic Pressure
- Definition: Pressure in the arteries during ventricular relaxation.
- Typical Value: ~80 mm Hg
- Significance: Indicates the force when the heart is at rest between beats.
-
Pulse Pressure
- Definition: The difference between systolic and diastolic pressures.
Pulse Pressure = Systolic Pressure−Diastolic Pressure
Ex: Pulse Pressure = 120mm Hg − 80mm Hg = 40mm Hg - Significance: Reflects the force that the heart generates each time it contracts.
- Definition: The difference between systolic and diastolic pressures.
-
Mean Arterial Pressure (MAP)
- Definition: Average pressure in the arteries during one cardiac cycle.
- Formula: MAP = Diastolic Pressure + 1/3 × Pulse Pressure
- Significance: Provides an overall indication of blood flow to organs.
Blood Pressure Regulation
Blood pressure is regulated by multiple mechanisms to maintain homeostasis, including:
-
Nervous System
- Sympathetic Nervous System: Increases heart rate and vasoconstriction.
- Parasympathetic Nervous System: Decreases heart rate.
-
Renal System
- Adjusts blood volume through regulation of kidney function.
- Renin-Angiotensin-Aldosterone System (RAAS): Increases blood pressure by retaining sodium and water.
-
Endocrine System
- ADH (Antidiuretic Hormone): Promotes water reabsorption in kidneys, increasing blood volume and pressure.
- Epinephrine and Norepinephrine: Increase heart rate and vasoconstriction.
-
Baroreceptors
- Located in the aortic arch and carotid sinuses.
- Detect changes in blood pressure and send signals to the brain to adjust heart rate and vessel diameter accordingly.
The Cardiac Cycle
The Cardiac Cycle encompasses all the events that occur during one heartbeat, including both electrical and mechanical activities.
Phases of the Cardiac Cycle
-
Ventricular Systole (0.33 sec)
-
Isovolumic Contraction (0.08 sec)
- Phase 1: Asynchronous Contraction (0.05 sec)
- Ventricular muscles begin to contract.
- AV valves close to prevent backflow into atria.
- SL valves remain closed.
- Ventricular volume remains unchanged; pressure increases.
- Phase 2: Isovolumic Contraction (0.03 sec)
- Continued ventricular contraction.
- Ventricular pressure rises sharply.
- SL valves remain closed until ventricular pressure exceeds arterial pressure.
- Phase 1: Asynchronous Contraction (0.05 sec)
-
Ejection Phase (0.25 sec)
- Phase 3: Rapid Ejection (0.12 sec)
- Ventricular pressure surpasses arterial pressure.
- SL valves open, allowing blood to be ejected rapidly.
- Ventricular volume decreases significantly.
- Phase 4: Reduced Ejection (0.13 sec)
- Ventricular pressure begins to decline.
- Ejection rate slows as arterial pressure approaches ventricular pressure.
- Ventricular volume continues to decrease at a slower rate.
- Phase 3: Rapid Ejection (0.12 sec)
-
-
Ventricular Diastole (0.47 sec)
-
Isovolumic Relaxation (0.12 sec)
- Phase 5: Protodiastole (0.04 sec)
- Ventricular muscles start to relax.
- SL valves remain open; AV valves stay closed.
- Ventricular volume remains constant.
- Phase 6: Isovolumic Relaxation (0.08 sec)
- Continued ventricular relaxation.
- Ventricular pressure drops rapidly.
- All valves remain closed; ventricular volume remains unchanged.
- Phase 5: Protodiastole (0.04 sec)
-
Filling Phase (0.35 sec)
- Phase 7: Rapid Filling (0.08 sec)
- Ventricular pressure falls below atrial pressure.
- AV valves open; blood flows rapidly from atria to ventricles.
- Ventricular volume increases sharply.
- Phase 8: Reduced Filling (0.17 sec)
- Filling rate decreases as ventricular pressure approaches atrial pressure.
- Ventricular volume continues to increase but at a slower rate.
- Phase 7: Rapid Filling (0.08 sec)
-
Presystole (0.1 sec)
- Phase 9: Presystole (0.1 sec)
- Atrial contraction (atrial systole) tops off ventricular filling.
- Ventricular volume increases slightly.
- Prepares the heart for the next cycle of systole.
- Phase 9: Presystole (0.1 sec)
-
Summary of Cardiac Cycle Phases
- Systole: Ventricular contraction and blood ejection.
- Diastole: Ventricular relaxation and filling.
- Total Duration: Approximately 0.8 seconds per cycle.
Factors Influencing Cardiac Output
-
Heart Rate (HR)
- Increased by: Sympathetic stimulation, exercise, stress.
- Decreased by: Parasympathetic stimulation, rest.
-
Stroke Volume (SV)
- Preload: The initial stretching of the cardiac myocytes prior to contraction; increased preload enhances SV.
- Afterload: The resistance the ventricles must overcome to eject blood; increased afterload can decrease SV.
- Contractility: The inherent vigor of the heart's contraction; increased contractility enhances SV.
-
Frank-Starling Law
- Principle: The heart pumps out more blood when it is filled with more blood during diastole (up to a physiological limit).
- Implication: Increased venous return (preload) leads to increased stroke volume.
Blood Pressure
Blood Pressure (BP) is the force exerted by circulating blood on the walls of blood vessels, primarily arteries. It is a critical indicator of cardiovascular health.
Types of Blood Pressure
-
Systolic Pressure
- Definition: The pressure in the arteries during ventricular contraction (systole).
- Typical Value: ~120 mm Hg
- Significance: Indicates the force the heart generates with each contraction.
-
Diastolic Pressure
- Definition: The pressure in the arteries during ventricular relaxation (diastole).
- Typical Value: ~80 mm Hg
- Significance: Reflects the residual pressure in the arteries when the heart is at rest.
-
Pulse Pressure
- Definition: The difference between systolic and diastolic pressures.
- Significance: Represents the force that the heart generates with each contraction; indicative of arterial stiffness.
-
Mean Arterial Pressure (MAP)
- Definition: The average pressure within the arterial system during one cardiac cycle.
- Significance: Reflects the average driving pressure for blood flow to organs.
Blood Pressure Regulation
Blood pressure is maintained through a combination of neural, hormonal, and local mechanisms:
-
Neural Regulation
- Sympathetic Nervous System: Increases heart rate and vasoconstriction, raising BP.
- Parasympathetic Nervous System: Decreases heart rate, lowering BP.
-
Hormonal Regulation
- Renin-Angiotensin-Aldosterone System (RAAS): Increases blood volume and systemic vascular resistance, elevating BP.
- Antidiuretic Hormone (ADH): Promotes water reabsorption in kidneys, increasing blood volume and BP.
- Epinephrine and Norepinephrine: Enhance heart rate and contractility, and cause vasoconstriction.
-
Local Regulation
- Baroreceptors: Stretch-sensitive receptors in the aortic arch and carotid sinuses detect BP changes and send signals to the brain to adjust heart rate and vessel diameter.
- Chemoreceptors: Detect changes in blood pH, CO₂, and O₂ levels, influencing respiratory and cardiovascular responses.
-
Frank-Starling Mechanism
- Adjusts stroke volume based on ventricular filling (preload) to help stabilize BP.
Clinical Relevance
- Hypertension (High Blood Pressure): Chronic elevation of BP, increasing the risk of heart disease, stroke, and kidney failure.
- Hypotension (Low Blood Pressure): Can lead to inadequate tissue perfusion and organ dysfunction.
- Pulse Pressure Changes: Elevated pulse pressure may indicate arterial stiffness or other cardiovascular issues.
Blood Vessel Structure
The structure of blood vessels is intricately designed to fulfill their specific functions in the circulatory system. Blood vessels are classified into arteries, arterioles, capillaries, venules, and veins, each with unique structural features.
Arteries
- Function: Transport blood away from the heart to various body parts.
- Structure:
- Thick, Muscular Walls: Composed of three layers—tunica intima, tunica media, and tunica externa.
- Tunica Intima: Inner endothelial lining.
- Tunica Media: Thick layer of smooth muscle and elastic fibers.
- Tunica Externa: Outer layer of connective tissue.
- Elasticity: Accommodates the surge of blood during systole and maintains pressure during diastole.
- Thick, Muscular Walls: Composed of three layers—tunica intima, tunica media, and tunica externa.
- Special Features:
- Aorta: Main artery carrying oxygenated blood from the left ventricle; highly elastic to absorb pulse pressure.
- Aorta: Main artery carrying oxygenated blood from the left ventricle; highly elastic to absorb pulse pressure.
Arterioles
- Function: Control blood flow into capillaries and regulate systemic vascular resistance.
- Structure:
- Smaller Diameter than Arteries: Less elastic, more muscular.
- Thinner Walls: Relative to arteries but sufficient for vasoconstriction and vasodilation.
- Role in MAP: Critical in maintaining Mean Arterial Pressure through resistance adjustments.
Capillaries
- Function: Facilitate exchange of gases, nutrients, and waste products between blood and tissues.
- Structure:
- Single-Cell Thick Walls: Endothelial cells allow easy diffusion.
- Small Diameter: Enables close proximity to tissue cells.
- Types:
- Continuous Capillaries: Tight junctions; limited permeability.
- Fenestrated Capillaries: Pores in endothelial cells; higher permeability.
- Sinusoidal Capillaries: Large gaps; allow passage of cells and large molecules.
Venules
- Function: Collect blood from capillaries and transport it to veins.
- Structure:
- Small Diameter Vessels: Larger than capillaries but smaller than veins.
- Thin Walls: Less muscular than arterioles.
Veins
- Function: Return deoxygenated blood to the heart from the body.
- Structure:
- Thin, Less Muscular Walls: Compared to arteries.
- Larger Lumens: Can hold more blood; act as blood reservoirs.
- Valves: Prevent backflow of blood, especially in the extremities.
- Special Features:
- Pulmonary Vein: Carries oxygenated blood from lungs to the left atrium; unique among veins as it carries oxygen-rich blood.
Blood Components
1. Red Blood Cells (Erythrocytes)
- Function: Transport oxygen and carbon dioxide.
- Characteristics:
- Shape: Biconcave discs increasing surface area for gas exchange.
- No Nucleus: Maximizes space for hemoglobin.
- Lifespan: Approximately 120 days; eventually removed by the spleen.
- Production: Erythropoiesis occurs in red bone marrow.
- Hemoglobin: Iron-containing protein responsible for oxygen binding.
- Oxyhemoglobin: Oxygen-bound hemoglobin appears bright red.
- Deoxyhemoglobin: Oxygen-released hemoglobin appears darker red.
2. White Blood Cells (Leukocytes)
- Function: Protect the body against infections and foreign invaders.
- Types:
- Neutrophils: Phagocytize bacteria and debris; most abundant leukocytes.
- Lymphocytes: B cells and T cells involved in adaptive immunity.
- Monocytes: Differentiate into macrophages; phagocytize pathogens and dead cells.
- Eosinophils: Combat parasitic infections and participate in allergic reactions.
- Basophils: Release histamine and heparin during allergic responses.
3. Platelets (Thrombocytes)
- Function: Essential for blood clotting and wound repair.
- Characteristics:
- Origin: Fragmented from megakaryocytes in the bone marrow.
- Action:
- Aggregation: Gather at injury sites to form platelet plugs.
- Clot Formation: Release clotting factors that initiate the coagulation cascade, leading to fibrin clot formation.
Cardiac Muscle Properties
Automaticity
- Definition: The heart's ability to generate its own electrical impulses.
- Pacemaker Locations:
- Sinoatrial (SA) Node: Primary pacemaker.
- Atrioventricular (AV) Node: Secondary pacemaker.
- Purkinje Fibers: Tertiary pacemaker.
Excitability
- Definition: The ability of cardiac cells to respond to stimuli by generating action potentials.
- Action Potential Phases in Contractile Cells:
- Phase 0 (Depolarization):
- Triggered when membrane potential reaches threshold (~-40 mV).
- Mechanism: Opening of voltage-gated fast Na⁺ channels allows rapid Na⁺ influx.
- Phase 1 (Initial Repolarization):
- Mechanism: Transient K⁺ efflux causes slight repolarization.
- Note: Na⁺ channels enter an inactivated state.
- Phase 2 (Plateau Phase):
- Mechanism: Balance between Ca²⁺ influx via voltage-gated channels and K⁺ efflux.
- Maintains depolarization for sustained contraction.
- Phase 3 (Repolarization):
- Mechanism: Closure of Ca²⁺ channels and increased K⁺ efflux leads to repolarization.
- Mechanism: Closure of Ca²⁺ channels and increased K⁺ efflux leads to repolarization.
- Phase 4 (Resting Membrane Potential):
- Mechanism: Active pumping of Na⁺ out and K⁺ into the cell restores resting potential.
- Phase 0 (Depolarization):
Conduction
- Intrinsic Conduction System
- Components: SA node → Atria → AV node → Bundle of His → Bundle Branches → Purkinje fibers.
- Function: Coordinates the electrical impulses leading to synchronized heart contractions.
Contraction
- Excitation-Contraction Coupling
- Initiation:
- Action potential initiated by pacemaker cells spreads through conduction pathways.
- Action potential initiated by pacemaker cells spreads through conduction pathways.
- Excitation:
- Action potential propagates along sarcolemma and enters T-tubules.
- Ca²⁺ Influx: Opens voltage-gated L-type Ca²⁺ channels, triggering Ca²⁺ release from the sarcoplasmic reticulum (SR) via ryanodine receptors (RyR).
- Contraction:
- Ca²⁺ binds to troponin, causing tropomyosin to shift and expose binding sites on actin.
- Cross-Bridge Cycling: Myosin heads attach to actin, perform power strokes, and generate contraction.
- Relaxation:
- Ca²⁺ is pumped back into the SR and extruded from the cell via the Na⁺/Ca²⁺ exchanger (NCX).
- Decreased intracellular Ca²⁺ leads to detachment of myosin from actin and sarcomere relaxation.
- Initiation:
Electrocardiography (ECG)
Electrocardiography (ECG) is a non-invasive diagnostic tool that records the electrical activity of the heart, providing valuable information about cardiac rhythm and function.
Components of ECG
-
Waves
- P Wave: Represents atrial depolarization.
- QRS Complex: Represents ventricular depolarization.
- T Wave: Represents ventricular repolarization.
- U Wave: Represents repolarization of papillary muscles or Purkinje fibers (rarely seen).
-
Segments
- PR Segment: Time between atrial and ventricular depolarization.
- ST Segment: Time between ventricular depolarization and repolarization.
-
Intervals
- PR Interval: From the start of the P wave to the start of the QRS complex.
- QT Interval: From the start of the QRS complex to the end of the T wave.
Interpretation of ECG
- Normal Sinus Rhythm: Regular rhythm initiated by the SA node.
- Arrhythmias: Irregularities in heart rhythm (e.g., atrial fibrillation, ventricular tachycardia).
- Ischemia and Infarction: Changes in the ECG can indicate reduced blood flow or damage to heart tissue.


Free Videos