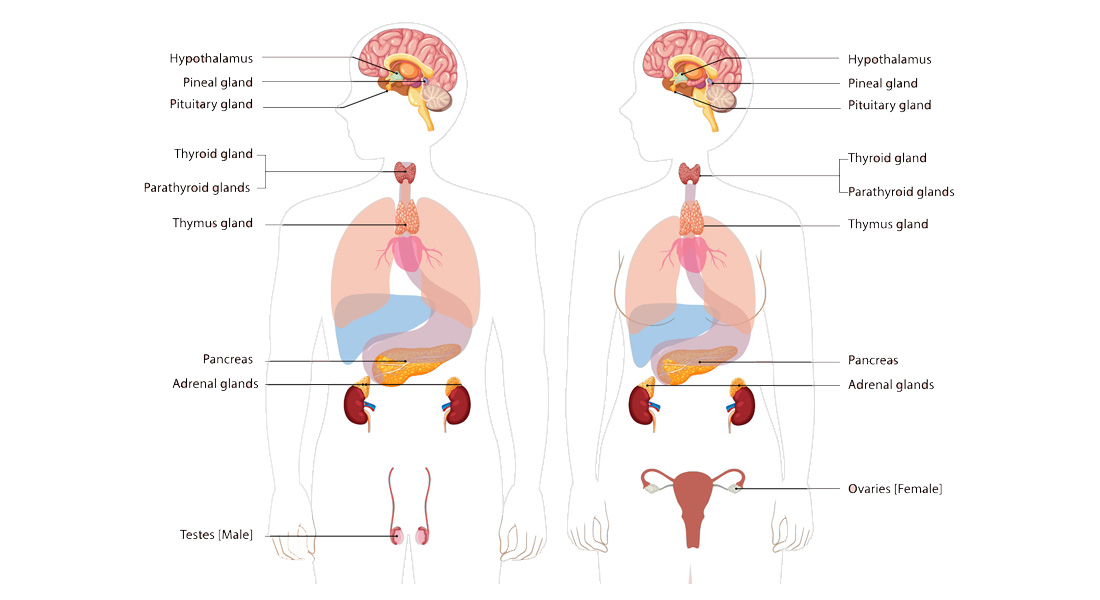
Endocrine Glands
The endocrine glands secrete hormones directly into the bloodstream and play a crucial role in regulating various body functions. One of the primary endocrine glands is the pituitary gland, often referred to as the master gland, due to its control over other endocrine glands. The pituitary gland works under the regulation of the hypothalamus and is suspended from the base of the brain near the 3rd ventricle.
Pituitary Gland (Hypophysis Cerebri)
- Small, reddish-grey, ovoid body about 12 mm in transverse diameter, weighing approximately 500 mg.
- Situated in the hypophyseal fossa, which is roofed by the diaphragma sellae, a part of the dura mater.
- It is composed of two main parts:
- Anterior Lobe (Adenohypophysis)
- Posterior Lobe (Neurohypophysis)
Anterior Lobe (Adenohypophysis)
- Embryological origin: Ectodermal derivative from the roof of the mouth (stomatodeum).
- It is made up of:
- Pars anterior (distalis), the largest part.
- Pars intermedia, a thin region that may fuse with the posterior lobe.
- Pars tuberalis, wrapping around the infundibulum.
Histology:
- Contains clusters of epithelial cells with reticular fibers.
- The cells are arranged in clumps or cords between fenestrated capillaries.
- Cell types:
- Chromophobe cells (50%) – inactive or degranulated cells with few granules.
- Chromophil cells (50%) – further divided into:
- Acidophils (40% of parenchyma):
- Somatotrophs secrete growth hormone (GH), which regulates growth.
- Mammotrophs secrete prolactin, essential for milk production.
- Basophils (10% of parenchyma):
- Thyrotrophs secrete thyroid-stimulating hormone (TSH).
- Gonadotrophs secrete follicle-stimulating hormone (FSH) and luteinizing hormone (LH).
- Corticotrophs secrete adrenocorticotropic hormone (ACTH) and lipotropin (LPH).
- Acidophils (40% of parenchyma):
Posterior Lobe (Neurohypophysis)
- Derived from a down-growth of the diencephalon and consists primarily of unmyelinated nerve fibers and pituicytes.
- Histology:
- The posterior lobe is not glandular but contains nerve fibers from the hypothalamus (supraoptic and paraventricular nuclei).
- Herring bodies are dilations of nerve fibers containing neurosecretory granules.
- Hormones:
- Vasopressin (ADH), which controls water reabsorption in the kidneys.
- Oxytocin, which promotes uterine contraction during childbirth and milk ejection during lactation.
Hypothalamic Control
The hypothalamus regulates the pituitary through neurosecretory cells, which release hormones into the hypophyseal portal system to stimulate or inhibit the secretion of hormones by the anterior pituitary.
Pituitary Hormones
- Anterior pituitary:
- ACTH, TSH, LH, FSH, Prolactin, GH, and MSH.
- Posterior pituitary:
- ADH and Oxytocin.
Endocrine Hormones and Conditions:
-
TRH (Thyrotropin-Releasing Hormone):
- Secreted by: Dorsomedial nucleus of the hypothalamus.
- Function: Stimulates the release of TSH from the anterior pituitary, which in turn stimulates the thyroid gland to produce thyroid hormones.
-
LHRH (Luteinizing Hormone-Releasing Hormone):
- Secreted by: Preoptic area & anterior hypothalamus.
- Function: Promotes the secretion of LH and FSH, important in reproductive health.
-
CRH (Corticotropin-Releasing Hormone):
- Secreted by: Supraoptic & paraventricular nuclei of the hypothalamus.
- Function: Stimulates the anterior pituitary to release ACTH, which influences adrenal gland hormone production.
-
GHRH (Growth Hormone-Releasing Hormone):
- Secreted by: Ventromedial nucleus.
- Function: Stimulates the release of growth hormone from the anterior pituitary.
-
GIH (Growth Inhibiting Hormone/Somatostatin):
- Secreted by: Periventricular nucleus.
- Function: Inhibits the release of growth hormone and TSH.
-
PRH (Prolactin-Releasing Hormone):
- Location: Not yet well-defined.
- Function: Promotes the release of prolactin for lactation.
-
PIH (Prolactin Inhibitory Hormone/Dopamine):
- Secreted by: Arcuate nucleus.
- Function: Dopamine acts to inhibit prolactin release.
Endocrine Disorders:
Dwarfism
- Definition: Slow or delayed growth leading to shorter stature.
- Clinical Features:
- Delayed puberty.
- Short arms and legs but an average-sized trunk.
- Disproportionately large head with a prominent forehead.
- Limited joint mobility.
- Adult height around 4 feet.
Gigantism
- Definition: Excessive growth due to overproduction of growth hormone before epiphyseal closure.
- Clinical Features:
- Very large hands and feet.
- Prominent jaw, coarse facial features, and thick fingers and toes.
- Height between 7 and 9 feet.
Acromegaly
- Definition: Excess growth hormone after the growth plates have closed.
- Clinical Features:
- Enlarged hands, feet, forehead, and jaw.
- Thicker skin, joint pain, and deepened voice.
- Complications may include diabetes, sleep apnea, and hypertension.
Pineal Gland
- Location: In the epithalamus, between the two hemispheres of the brain.
- Function: Produces melatonin, regulating sleep-wake cycles and seasonal rhythms.
- Histology:
- Pinealocytes: Produce melatonin.
- Interstitial cells: Provide structural support.
- Perivascular phagocytes: Serve an immune function.
Thyroid Gland
- Location: Front of the neck, below the Adam's apple.
- Function: Secretes thyroid hormones:
- Triiodothyronine (T3) and Thyroxine (T4), which regulate metabolism.
- Calcitonin, which regulates calcium levels.
- Histology:
- Follicles: Spherical groups of cells surrounding a colloid core.
- Follicular cells: Produce thyroid hormones.
- Parafollicular cells: Secrete calcitonin.
Thyroid Gland Structure & Function
Follicular Cells:
- These cells form a single layer around the core of a thyroid follicle.
- When stimulated by Thyroid Stimulating Hormone (TSH), they produce and secrete the thyroid hormones Triiodothyronine (T3) and Thyroxine (T4).
- The process involves transporting thyroglobulin from the colloid into the cell, metabolizing it, and releasing active thyroid hormones.
- The shape of these cells varies based on their activity level—ranging from flat to cuboid or columnar.
Parafollicular Cells (C Cells):
- Found scattered among follicular cells and in spaces between follicles.
- Their primary role is to secrete calcitonin, which helps regulate calcium homeostasis by lowering blood calcium levels when they are high.
Thyroid Gland Anatomy
- The thyroid gland typically weighs 10 to 20 grams in adults, with volume slightly greater in men than in women.
- The size of the gland increases with age and body weight but decreases with higher iodine intake.
- It is one of the most vascular organs, making it prone to size variations during procedures like surgery.
Location & Relations:
- Positioned just below the larynx, encircling the anterolateral portion of the trachea.
- Medially bordered by the trachea and esophagus, and laterally by the carotid sheath.
- Anterior and lateral relations include the sternocleidomastoid muscle and strap muscles (sternohyoid, sternothyroid, and the superior belly of the omohyoid).
Shape:
- Consists of two lobes connected by a narrow isthmus.
- Each lobe has a pyramidal shape, with the apex directed upwards and the base downwards.
- Occasionally, a small pyramidal lobe extends from the isthmus, usually left of the midline.
Blood Supply
-
Superior Thyroid Artery:
- Branches from the external carotid artery and supplies the superior pole of the thyroid.
- It also supplies approximately 15% of the superior parathyroid glands.
-
Inferior Thyroid Artery:
- A branch of the thyrocervical trunk (arising from the subclavian artery).
- It enters the lateral side of the thyroid and supplies both inferior parathyroid glands and 85% of superior parathyroid glands.
-
Thyroidea Ima Artery (present in 3% of individuals):
- Arises from the aortic arch or innominate artery.
- Important in surgeries like thyroidectomy as it can be enlarged in thyroid diseases like goiter or hyperthyroidism.
Venous Drainage
- Superior Thyroid Vein: Drains the upper part of the thyroid and empties into the internal jugular vein.
- Middle Thyroid Vein: Drains the middle of the thyroid lobe, also ending in the internal jugular vein.
- Inferior Thyroid Veins: Drain the lower parts of the lobes and isthmus, emptying into the left brachiocephalic vein.
Lymphatic Drainage
- Lymphatic vessels from the thyroid gland drain into the pretracheal and paratracheal lymph nodes.
- Efferent vessels from these nodes further drain into the deep cervical lymph nodes.
Thyroid Physiology
Synthesis of Thyroid Hormones:
- Iodide Trapping: The follicular cells actively transport inorganic iodide from the blood.
- Oxidation: Iodide is oxidized into iodine within the follicular cells.
- Iodination: Iodine binds to tyrosine residues in the thyroglobulin to form iodotyrosines.
- Coupling: Mono-iodotyrosines (MIT) and di-iodotyrosines (DIT) combine to form T3 and T4.
- T3 is formed by one MIT and one DIT, while T4 is formed by two DITs.
Metabolic Effects of Thyroid Hormones:
- T3 is the more active hormone and can be produced in peripheral tissues by converting T4 into T3.
- T3 acts quickly (within hours), while T4 takes longer to act (4-14 days).
Functions of Thyroid Hormones:
- Metabolic: Regulate the body's metabolic rate by increasing oxygen consumption and heat production.
- Cardiovascular: Increase heart rate and cardiac output by enhancing the response to catecholamines.
- Developmental: Essential for normal growth and development, particularly in the nervous system.
Regulation of Thyroid Hormone Production
-
Thyrotropin-Releasing Hormone (TRH):
- TRH is secreted by the hypothalamus and stimulates the anterior pituitary gland to release Thyroid Stimulating Hormone (TSH).
- TSH in turn stimulates the thyroid gland to produce and release T3 (triiodothyronine) and T4 (thyroxine).
-
Negative Feedback Mechanism:
- Both T3 and T4 inhibit further secretion of TSH by providing negative feedback to the pituitary gland and hypothalamus. This helps maintain balance in thyroid hormone levels.
- The liver and other tissues convert T4 to the more active T3 through the enzyme T4 monodeiodinase.
-
Metabolism and Excretion:
- Some T4 and T3 are conjugated with glucuronide and sulfate in the liver. They are then excreted in the bile and partially hydrolyzed in the intestine.
- Some of the hormones can be reabsorbed from the intestine through a process known as enterohepatic circulation.
-
Drug Interactions:
- Drug interactions can occur at various steps in this process, including hormone synthesis, conversion, and reabsorption.
Effects of Thyroid Hormones
- Fetal Development: Essential for brain and skeletal maturation during fetal development.
- Metabolism: Increases basal metabolic rate, promoting energy production and heat generation.
- Catecholamine Sensitivity: Enhances sensitivity to catecholamines like adrenaline, influencing heart rate and nervous system activity.
- Digestive System: Stimulates gut motility.
- Bone Health: Increases bone turnover, helping to maintain bone density.
- Glucose and Cholesterol: Increases serum glucose levels and reduces serum cholesterol, contributing to overall metabolism.
Applied Anatomy and Physiology
-
Hypothyroidism:
- A condition where the thyroid gland does not produce sufficient thyroid hormones.
- Symptoms include fatigue, weight gain, cold intolerance, and slow heart rate.
-
Hyperthyroidism:
- Overproduction of thyroid hormones, leading to an overactive metabolism.
- Symptoms include weight loss, rapid heart rate, tremors, and sweating.
-
Thyroiditis:
- Inflammation of the thyroid gland, often leading to thyroid dysfunction.
- Inflammation of the thyroid gland, often leading to thyroid dysfunction.
-
Thyroid Cancer:
- Malignancy affecting the thyroid gland, typically treated through surgery and radiotherapy.
- Malignancy affecting the thyroid gland, typically treated through surgery and radiotherapy.
-
Goiter:
- Enlargement of the thyroid gland, which can be associated with both hyperthyroidism and hypothyroidism.
- Enlargement of the thyroid gland, which can be associated with both hyperthyroidism and hypothyroidism.
-
Cretinism:
- A severe form of congenital hypothyroidism that results in stunted physical and mental development. It is commonly caused by iodine deficiency during pregnancy.
Parathyroid Glands
- The parathyroid glands are four small glands located behind the thyroid that regulate calcium levels in the body through the secretion of parathyroid hormone (PTH).
Functions of Parathyroid Hormone (PTH):
- Regulates calcium by acting on bones, kidneys, and the intestines.
- Decreases phosphate reabsorption in the kidneys.
- Activates Vitamin D: PTH increases the activity of 1-α-hydroxylase, converting inactive Vitamin D into its active form, 1,25-dihydroxycholecalciferol.
Blood Supply:
- The superior parathyroid glands are primarily supplied by the inferior thyroid artery, with some contribution from the superior thyroid artery.
- The inferior parathyroid glands are supplied by the inferior thyroid artery.
Stimulants:
- Low calcium levels in the blood stimulate the secretion of PTH.
- Low magnesium levels and increased phosphate levels can also trigger PTH secretion.
Inhibitors:
- High calcium levels inhibit PTH secretion.
- Severe magnesium deficiency can suppress PTH activity.
Pancreas Anatomy
The pancreas is a J-shaped gland with both exocrine and endocrine functions. It is located in the epigastric and left hypochondriac regions behind the stomach and across the posterior abdominal wall.
Key Components:
-
Head:
- Lies in the concavity of the duodenum with its borders defined by surrounding organs.
- Lies in the concavity of the duodenum with its borders defined by surrounding organs.
-
Neck:
- Located between the head and the body, it is related to the pylorus anteriorly and the superior mesenteric vein and portal vein posteriorly.
- Located between the head and the body, it is related to the pylorus anteriorly and the superior mesenteric vein and portal vein posteriorly.
-
Body:
- Extends to the left with borders related to the transverse mesocolon, coeliac trunk, hepatic, and splenic arteries.
- Extends to the left with borders related to the transverse mesocolon, coeliac trunk, hepatic, and splenic arteries.
-
Tail:
- Lies in the lienorenal ligament and is associated with the spleen.
Duct System:
- The main pancreatic duct of Wirsung runs through the body and opens into the duodenum via the hepatopancreatic ampulla of Vater.
- The accessory duct of Santorini may also open into the duodenum through the minor duodenal papilla.
Thyroid hormone synthesis
The synthesis of thyroid hormones (T3 and T4) is a multi-step process that takes place within the thyroid gland, primarily in the follicular cells.
1. Iodide Trapping:
- Iodine uptake from the bloodstream is the first step. Iodide (I⁻) is actively transported into the follicular cells of the thyroid gland via a sodium/iodide symporter (NIS). This process is stimulated by Thyroid-Stimulating Hormone (TSH).
2. Oxidation of Iodide to Iodine:
- Once inside the follicular cells, iodide is oxidized to iodine by the enzyme thyroid peroxidase (TPO) at the apical membrane. This conversion is essential for the incorporation of iodine into the precursor protein, thyroglobulin.
3. Organification of Iodine:
- The iodine binds to tyrosine residues within thyroglobulin (a large glycoprotein produced by follicular cells). This results in the formation of monoiodotyrosine (MIT) and diiodotyrosine (DIT), a process known as iodination or organification. This is also catalyzed by thyroid peroxidase (TPO).
4. Coupling of Iodotyrosines:
- Two iodinated tyrosine residues then couple together to form thyroid hormones:
- DIT + DIT → Thyroxine (T4)
- DIT + MIT → Triiodothyronine (T3)
- This coupling reaction is also catalyzed by thyroid peroxidase (TPO) and occurs within the colloid of the thyroid follicles.
5. Storage of Thyroid Hormones:
- Once synthesized, the newly formed T3 and T4 remain bound to thyroglobulin in the colloid. The thyroid gland stores these hormones in this form until they are needed.
6. Endocytosis of Thyroglobulin:
- Upon stimulation by TSH, the follicular cells engulf the thyroglobulin containing T3 and T4 through endocytosis, bringing it back into the follicular cells from the colloid.
7. Proteolysis and Release:
- Inside the follicular cells, the thyroglobulin is broken down in lysosomes, releasing free T3 and T4 into the bloodstream. The majority of hormone released is T4, with smaller amounts of T3.
- T3 is the more biologically active form, and much of the T4 released is converted to T3 in peripheral tissues (like the liver and kidneys) through the action of the enzyme deiodinase.
8. Secretion into Bloodstream:
- T3 and T4 are secreted into the bloodstream, where they are mostly bound to plasma proteins like thyroxine-binding globulin (TBG), with only a small percentage circulating as free, active hormones.


Free Videos