Introduction to Excretion
Excretion is the physiological process by which the body eliminates unwanted substances and metabolic wastes. This vital function maintains homeostasis and ensures the removal of toxins and by-products of metabolism.
Major Excretory Systems and Their Functions
-
Digestive System
- Excretory Products: Eliminates food residues as feces.
- Additional Excretions: Removes some bacteria and toxic substances.
-
Respiratory System (Lungs)
- Excretory Products: Expels carbon dioxide and water vapor.
- Excretory Products: Expels carbon dioxide and water vapor.
-
Integumentary System (Skin)
- Excretory Products: Releases water, salts, and some waste products.
- Additional Function: Regulates body temperature by removing heat.
-
Hepatic System (Liver)
- Excretory Products: Produces bile, which excretes bile pigments, heavy metals, drugs, toxins, and bacteria.
Functions of the Kidney
The kidneys play a crucial role in maintaining the body's internal environment through several key functions:
- Excretion of Waste Products
- Maintenance of Water Balance
- Maintenance of Electrolyte Balance
- Maintenance of Acid–Base Balance
- Hemopoietic Function (Production of blood cells)
- Regulation of Blood Calcium Levels
Anatomy of the Kidney
-
Number and Location
- Two kidneys are present in all mammals.
- Located retroperitoneally at the level of the lower ribs.
- Protection: Shielded by the 11th and 12th ribs.
-
Positional Differences
- The left kidney is slightly more anterior compared to the right kidney.
- The left kidney is slightly more anterior compared to the right kidney.
-
Structural Regions
- Outer Region: Cortex (darker area).
- Inner Region: Medulla (lighter area) containing:
- Calyces: Major and minor.
- Renal Pyramids
- Renal Pelvis
- Blood Vessels
Nephron: Structural and Functional Unit of the Kidney
-
Definition: A nephron is the basic structural and functional unit of the kidney responsible for filtering blood and forming urine.
-
Quantity: Approximately 2,400,000 nephrons are present collectively in both kidneys.
-
Components of a Nephron
- Renal Corpuscle: Site of blood filtration.
- Renal Tubule: Transforms filtrate into urine as it moves toward the renal pelvis.
Types of Nephrons
-
Cortical Nephrons (Superficial Nephrons)
- Location: Corpuscles reside in the outer cortex near the kidney's periphery.
- Prevalence: Constitute about 85% of nephrons in human kidneys.
-
Juxtamedullary Nephrons
- Location: Corpuscles located in the inner cortex near the medulla (corticomedullary junction).
- Function: Possess longer loops of Henle, extending deep into the inner medulla, crucial for urine concentration.
Detailed Structure of a Nephron
- Bowman's Capsule
- Proximal Convoluted Tubule (PCT)
- Loop of Henle
- Descending Limb
- Ascending Limb
- Distal Convoluted Tubule (DCT)
- Collecting Tubule
- Collecting Duct
Renal Corpuscle
-
Glomerulus
- Description: A tuft of capillaries within Bowman's capsule.
- Blood Flow: Receives blood via the afferent arteriole and exits through the efferent arteriole.
- Vascular Nature: Purely arterial.
-
Bowman's Capsule
- Structure: Encloses the glomerulus, resembling a funnel with filter paper.
- Layers:
- Inner Visceral Layer
- Outer Parietal Layer
Tubular Portion of the Nephron
-
Proximal Convoluted Tubule (PCT)
- Location: Situated in the cortex.
- Structure: Coiled segment extending from Bowman's capsule.
- Continuation: Becomes the descending limb of the loop of Henle.
- Dimensions: Approximately 14 mm in length and 55 μm in diameter.
-
Loop of Henle
-
Components:
- Descending Limb:
- Segments:
- Thick Descending Segment: Direct continuation of the PCT; 6 mm long, 55 μm diameter.
- Thin Descending Segment: Follows the thick segment.
- Function: Permeable to water, allowing its reabsorption into the medulla.
- Segments:
- Hairpin Bend: Connects descending to ascending limb; formed by flattened epithelial cells without a brush border.
- Ascending Limb:
- Segments:
- Thin Ascending Segment
- Thick Ascending Segment: Approximately 9 mm long, 30 μm diameter.
- Macula Densa: Terminal portion located between afferent and efferent arterioles, part of the juxtaglomerular apparatus.
- Function: Impermeable to water; actively transports sodium and chloride out of the tubule.
- Segments:
- Descending Limb:
-
Variations:
- Cortical Nephrons: Have shorter loops extending only into the outer medulla.
- Juxtamedullary Nephrons: Possess longer loops reaching deep into the inner medulla, essential for concentrating urine.
-
-
Distal Convoluted Tubule (DCT)
- Location: Located in the cortex.
- Structure: Continues from the thick ascending limb of the loop of Henle.
- Dimensions: 14.5 to 15 mm in length, 22 to 50 μm in diameter.
- Function: Further adjusts the composition of the filtrate through selective reabsorption and secretion.
-
Collecting Duct
- Structure: Formed by principal (P) cells and intercalated (I) cells.
- Pathway:
- Begins in the cortex as the initial or arched collecting duct.
- Merges into straight collecting ducts passing through the medulla.
- Function: Final modification of urine concentration under hormonal control (e.g., ADH).
Regulation of Renal Blood Flow
Renal Autoregulation
- Purpose: Maintains a consistent glomerular filtration rate (GFR) despite fluctuations in systemic blood pressure (60 mm Hg to 180 mm Hg).
- Mechanisms:
- Myogenic Response: Vascular smooth muscle responds to pressure changes by constricting or dilating.
- Tubulo-Glomerular Feedback: Adjusts afferent arteriole resistance based on sodium chloride concentration at the macula densa.
Renin-Angiotensin System
- Role: Regulates systemic blood pressure and renal blood flow through hormone secretion.
Secretion of Hormones by the Juxtaglomerular Apparatus
-
Renin
- Type: Peptide hormone with 340 amino acids.
- Function: Initiates the renin-angiotensin-aldosterone system (RAAS), crucial for blood pressure regulation.
- Stimulation Factors:
- Decreased arterial blood pressure.
- Reduced extracellular fluid (ECF) volume.
- Increased sympathetic nervous activity.
- Decreased sodium and chloride load at the macula densa.
-
Prostaglandin
- Function: Modulates renal blood flow and GFR.
Actions of Angiotensins
- Angiotensin I: Inactive precursor.
- Angiotensin II: Active form with two primary actions:
- Vasoconstriction: Directly constricts arterioles, increasing blood pressure.
- Sympathetic Activation: Enhances noradrenaline release, promoting vasoconstriction.
Urine Formation
Urine formation involves three primary processes:
- Glomerular Filtration
- Tubular Reabsorption
- Tubular Secretion
Glomerular Filtration
-
Definition: The process of filtering blood plasma through the glomerular capillaries into Bowman's capsule.
-
Filtration Membrane Structure:
- Glomerular Capillary Membrane: Single layer with pores/fenestrations.
- Basement Membrane: Separates capillary endothelium from Bowman's capsule.
- Visceral Layer of Bowman's Capsule: Composed of podocytes with slit pores.
-
Ultrafiltration:
- Description: High-efficiency filtration allowing minute particles while retaining larger molecules like plasma proteins.
- Outcome: Filtrate contains plasma components except proteins.
-
Glomerular Filtration Rate (GFR)
- Definition: Volume of filtrate formed per minute (125 mL/min; ~180 L/day).
- Definition: Volume of filtrate formed per minute (125 mL/min; ~180 L/day).
-
Filtration Fraction
- Definition: Ratio of GFR to renal plasma flow, expressed as a percentage.
- Definition: Ratio of GFR to renal plasma flow, expressed as a percentage.
-
Determining Pressures for Filtration
- Glomerular Capillary Pressure
- Colloidal Osmotic Pressure in Glomeruli
- Hydrostatic Pressure in Bowman's Capsule
-
Net Filtration Pressure (Starling Hypothesis)
- Formula: Net Filtration = Hydrostatic Pressure Difference - Oncotic Pressure Difference
- Implication: Determines the net movement of fluid across the filtration membrane.
-
Factors Regulating GFR
- Renal Blood Flow
- Tubulo-Glomerular Feedback
- Glomerular Capillary Pressure
- Colloidal Osmotic Pressure
- Hydrostatic Pressure in Bowman's Capsule
- Constriction of Afferent Arteriole
- Constriction of Efferent Arteriole
- Systemic Arterial Pressure
- Sympathetic Stimulation
- Surface Area of Capillary Membrane
- Permeability of Capillary Membrane
- Hormonal and Other Factors
Tubular Reabsorption
-
Definition: Transport of water and solutes from the renal tubules back into the bloodstream.
-
Extent: Over 99% of filtrate is reabsorbed.
-
Routes of Reabsorption:
- Transcellular Route: Through the cells of the tubule.
- Paracellular Route: Between the cells of the tubule.
-
Sites and Substances Reabsorbed:
- Proximal Convoluted Tubule
- Substances: Glucose, amino acids, sodium, potassium, calcium, bicarbonates, chlorides, phosphates, urea, uric acid, water.
- Loop of Henle
- Substances: Sodium and chloride.
- Distal Convoluted Tubule
- Substances: Sodium, calcium, bicarbonate, and water.
- Substances: Sodium, calcium, bicarbonate, and water.
- Proximal Convoluted Tubule
-
Regulation of Tubular Reabsorption
- Glomerulo-Tubular Balance
- Hormonal Factors
- Nervous Factors
Tubular Secretion
- Definition: Movement of substances from the blood into the renal tubules.
- Excreted Substances:
- Para-aminohippuric acid (PAH)
- Diodrast
- 5-Hydroxyindoleacetic acid (5HIAA)
- Amino derivatives
- Penicillin
Summary of Urine Formation
- Glomerular Filtration: Plasma is filtered in the glomeruli, forming filtrate.
- Tubular Reabsorption: Approximately 99% of the filtrate is reabsorbed in the renal tubules.
- Tubular Secretion: Specific substances are secreted into the tubules from the blood.
Concentration and Dilution of Urine
Factors Influencing Urine Osmolarity
- Water Content in the Body
- Antidiuretic Hormone (ADH) Levels
Formation of Dilute Urine
- Condition: Increased water content in the body.
- Mechanism:
- ADH Inhibition: Reduced secretion from the posterior pituitary.
- Effect: Decreased water reabsorption from the renal tubules, leading to excretion of large volumes of dilute urine.
Formation of Concentrated Urine
- Condition: Decreased water content in the body.
- Mechanisms:
- Medullary Gradient Development: Maintained by the countercurrent system.
- ADH Secretion: Enhances water reabsorption in the collecting ducts.
Medullary Gradient
- Components of the Countercurrent System:
- Countercurrent Multiplier: Created by the loop of Henle.
- Countercurrent Exchanger: Formed by the vasa recta.
Role of ADH (Antidiuretic Hormone)
- Function: Increases the permeability of the distal convoluted tubule and collecting duct to water, promoting water reabsorption.
- Result: Concentrated urine with higher osmolarity (up to 1,200 mOsm/L).
Summary of Urine Concentration Process
- Bowman's Capsule: Filtrate is isotonic to plasma (300 mOsm/L).
- Proximal Convoluted Tubule: Active reabsorption of sodium and chloride; obligatory water reabsorption.
- Thick Descending Limb of Henle: Water reabsorption into the medulla due to high osmolarity (450-600 mOsm/L).
- Thin Descending Limb:
- Cortical Nephrons: Osmolarity reaches 600 mOsm/L.
- Juxtamedullary Nephrons: Osmolarity reaches 1,200 mOsm/L.
- Thin Ascending Limb of Henle: Sodium and chloride are reabsorbed, reducing osmolarity to ~400 mOsm/L.
- Thick Ascending Limb: Active reabsorption of sodium and chloride without water loss, lowering osmolarity to 150-200 mOsm/L.
- Distal Convoluted Tubule and Collecting Duct:
- With ADH: Increased water reabsorption, concentrating urine to 1,200 mOsm/L.
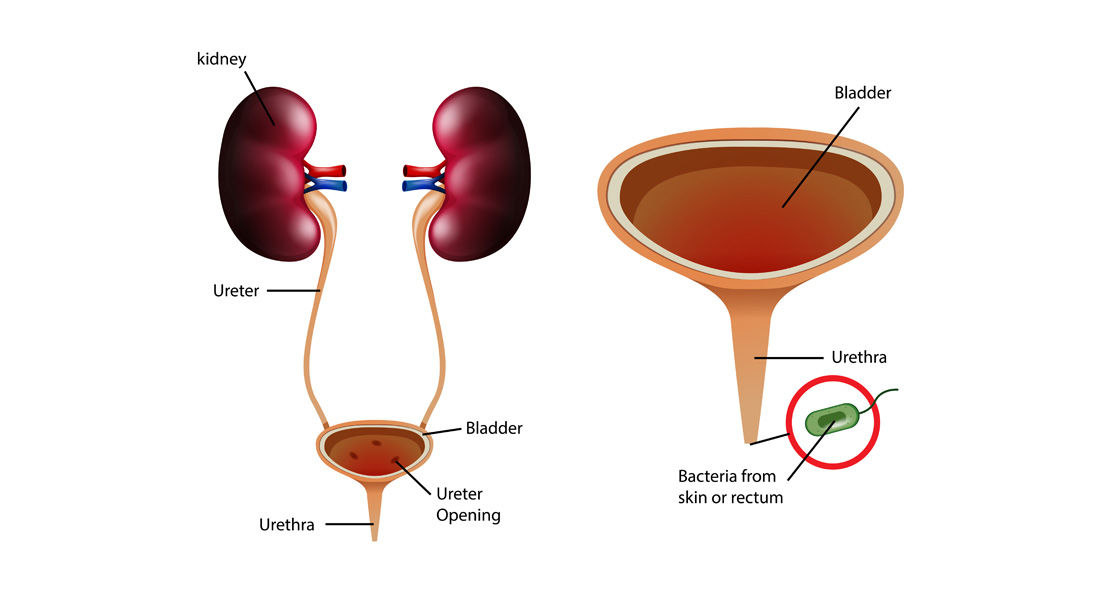
Micturition (Urination)
Process Overview
- Definition: The voiding of urine from the urinary bladder.
- Nature: Reflexive process, but voluntary control is possible in adults.
Urinary Bladder and Urethra
-
Urinary Bladder
- Location: Lower abdomen.
- Structure: Hollow, triangular organ with a body and neck.
- Wall Composition: Smooth muscle (detrusor muscle) with three layers:
- Inner longitudinal layer
- Middle circular layer
- Outer longitudinal layer
-
Urethral Sphincters
- Internal Urethral Sphincter: Involuntary control.
- External Urethral Sphincter: Voluntary control.
Nerve Supply
- Urinary Bladder and Sphincters: Innervated by the autonomic and somatic nervous systems, coordinating the micturition reflex.
Micturition Reflex
- Mechanism: Coordination between the nervous system and the smooth muscles of the bladder and sphincters to expel urine.
Properties of Urine
- Volume: 1,000 to 1,500 mL/day.
- Reaction: Slightly acidic (pH 4.5 to 6).
- Specific Gravity: 1.010 to 1.025.
- Osmolarity: 1,200 mOsm/L.
- Color: Typically straw-colored.
- Odor: Fresh urine has a light aromatic odor.


Free Videos